Recommendations
ACC/AHA/SCAI PCI Guidelines - British Cardiovascular Intervention ...
ACC/AHA/SCAI PCI Guidelines - British Cardiovascular Intervention ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
60<br />
Smith et al. 2005<br />
ACC/AHA/SCAI Practice Guidelines<br />
ACC - www.acc.org<br />
AHA - www.americanheart.org<br />
SCAI - www.scai.org<br />
the microcirculation or on the absolute magnitude of the<br />
change in coronary flow.<br />
On the other hand, CVR is the ratio of hyperemic to basal<br />
flow and reflects flow resistance through the epicardial<br />
artery and the microvascular bed. CVR less than 2.0 is positively<br />
correlated to abnormal stress perfusion imaging (632-<br />
634). In some cases, the uncertainty as to whether the<br />
impaired flow reserve is due to the target stenosis or to an<br />
abnormal microcirculation may be reduced by use of relative<br />
coronary flow reserve (rCVR, which is equal to CVR of the<br />
target vessel divided by CVR of the reference vessel). From<br />
preliminary studies, rCVR greater than 0.8 may have prognostic<br />
values similar to those of negative stress testing (635).<br />
There is a correlation between rCVR and pressure-derived<br />
FFR (629,635). An abnormal CVR indicates that the stenosis<br />
in the epicardial artery is significant when the microcirculation<br />
is normal. For coronary lesion assessment, the best<br />
measurement appears to be FFR.<br />
CVR measurement of less than 2 after stent placement was<br />
an independent predictor of target-vessel revascularization.<br />
CVR after PCI in DEBATE-2 (Doppler Endpoints Balloon<br />
Angioplasty Trial Europe) also predicted early MACE due to<br />
microcirculatory disturbances (636). However, because of<br />
the complexity in the interpretation of CVR, pressurederived<br />
FFR is the preferred measurement for lesion assessment<br />
and outcome of PCI. Coronary physiologic measurements<br />
associated with major clinical outcomes are supported<br />
by numerous studies (Table 23) (632,637).<br />
Strong correlations exist between myocardial stress testing<br />
and FFR or CVR (633,638-649). An FFR of less than 0.75<br />
identified physiologically significant stenoses associated<br />
with inducible myocardial ischemia with high sensitivity<br />
(88%), specificity (100%), positive predicted value (100%),<br />
and overall accuracy (93%). An abnormal CVR (less than<br />
2.0) corresponded to reversible myocardial perfusion imaging<br />
defects with high sensitivity (86% to 92%), specificity<br />
(89% to 100%), predictive accuracy (89% to 96%), and positive<br />
and negative predictive values (84% to 100% and 77%<br />
to 95%, respectively).<br />
The clinical outcomes of deferring coronary intervention<br />
for intermediate stenoses with normal physiology are<br />
remarkably consistent, with clinical event rates of less than<br />
10% over a 2-year follow-up period (639,647-651). Bech et<br />
al. (649) studied 325 patients with intermediate coronary<br />
stenosis without documented myocardial ischemia and randomly<br />
assigned those with FFR greater than 0.75 to a deferral<br />
group of 91 patients or a performance group of 90<br />
patients. PTCA was performed as planned in 144 patients<br />
with FFR less than 0.75. At clinical follow-up of 1, 3, 6, 12,<br />
and 24 months, event-free survival was similar between the<br />
deferral and performance groups (92% vs 89% at 12 months<br />
and 89% vs 83% at 24 months). However, these rates were<br />
significantly lower in the reference (PTCA) group (80% at<br />
12 months and 78% at 24 months). The percentage of<br />
patients free from angina was similar between the deferral<br />
and the performance group at 12 and 24 months, but there<br />
was a significantly higher incidence of angina in the refer-<br />
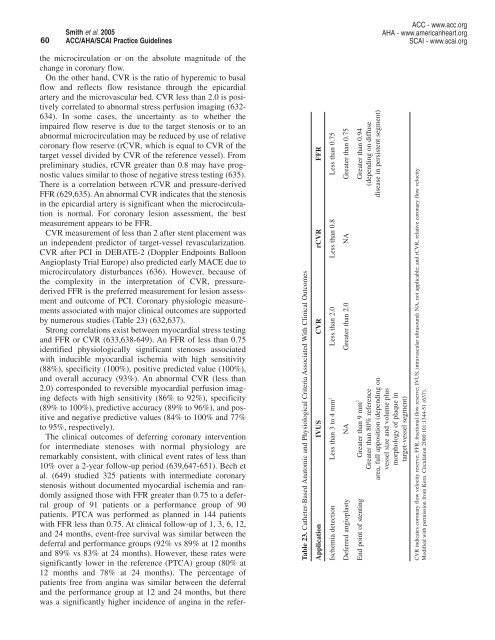
Table 23. Catheter-Based Anatomic and Physiological Criteria Associated With Clinical Outcomes<br />
Application IVUS CVR rCVR FFR<br />
Ischemia detection Less than 3 to 4 mm 2 Less than 2.0 Less than 0.8 Less than 0.75<br />
Deferred angioplasty NA Greater than 2.0 NA Greater than 0.75<br />
End point of stenting Greater than 9 mm 2 Greater than 0.94<br />
Greater than 80% reference (depending on diffuse<br />
area, full apposition (depending on disease in persistent segment)<br />
vessel size and volume plus<br />
morphology of plaque in<br />
target-vessel segment)<br />
CVR indicates coronary flow velocity reserve; FFR, fractional flow reserve; IVUS, intravascular ultrasound; NA, not applicable; and rCVR, relative coronary flow velocity.<br />
Modified with permission from Kern. Circulation 2000;101:1344-51 (637).