Recommendations
ACC/AHA/SCAI PCI Guidelines - British Cardiovascular Intervention ...
ACC/AHA/SCAI PCI Guidelines - British Cardiovascular Intervention ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ACC - www.acc.org<br />
AHA - www.americanheart.org<br />
SCAI - www.scai.org<br />
Smith et al. 2005<br />
ACC/AHA/SCAI Practice Guidelines<br />
67<br />
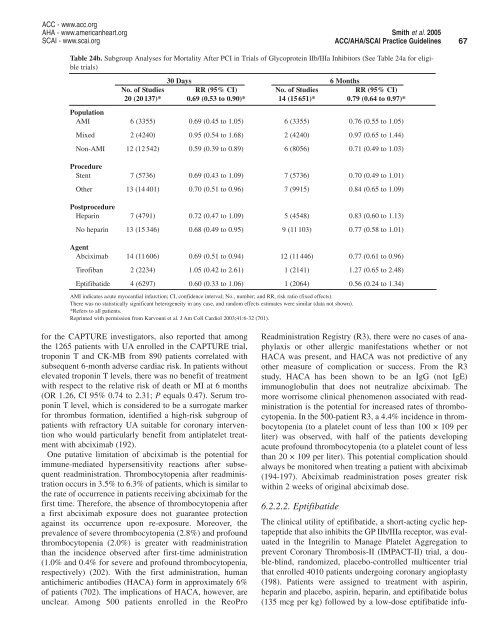
Table 24b. Subgroup Analyses for Mortality After PCI in Trials of Glycoprotein IIb/IIIa Inhibitors (See Table 24a for eligible<br />
trials)<br />
30 Days 6 Months<br />
No. of Studies RR (95% CI) No. of Studies RR (95% CI)<br />
20 (20 137)* 0.69 (0.53 to 0.90)* 14 (15 651)* 0.79 (0.64 to 0.97)*<br />
Population<br />
AMI 6 (3355) 0.69 (0.45 to 1.05) 6 (3355) 0.76 (0.55 to 1.05)<br />
Mixed 2 (4240) 0.95 (0.54 to 1.68) 2 (4240) 0.97 (0.65 to 1.44)<br />
Non-AMI 12 (12 542) 0.59 (0.39 to 0.89) 6 (8056) 0.71 (0.49 to 1.03)<br />
Procedure<br />
Stent 7 (5736) 0.69 (0.43 to 1.09) 7 (5736) 0.70 (0.49 to 1.01)<br />
Other 13 (14 401) 0.70 (0.51 to 0.96) 7 (9915) 0.84 (0.65 to 1.09)<br />
Postprocedure<br />
Heparin 7 (4791) 0.72 (0.47 to 1.09) 5 (4548) 0.83 (0.60 to 1.13)<br />
No heparin 13 (15 346) 0.68 (0.49 to 0.95) 9 (11 103) 0.77 (0.58 to 1.01)<br />
Agent<br />
Abciximab 14 (11 606) 0.69 (0.51 to 0.94) 12 (11 446) 0.77 (0.61 to 0.96)<br />
Tirofiban 2 (2234) 1.05 (0.42 to 2.61) 1 (2141) 1.27 (0.65 to 2.48)<br />
Eptifibatide 4 (6297) 0.60 (0.33 to 1.06) 1 (2064) 0.56 (0.24 to 1.34)<br />
AMI indicates acute myocardial infarction; CI, confidence interval; No., number; and RR, risk ratio (fixed effects).<br />
There was no statistically significant heterogeneity in any case, and random effects estimates were similar (data not shown).<br />
*Refers to all patients.<br />
Reprinted with permission from Karvouni et al. J Am Coll Cardiol 2003;41:6-32 (701).<br />
The clinical utility of eptifibatide, a short-acting cyclic heptapeptide<br />
that also inhibits the GP IIb/IIIa receptor, was evaluated<br />
in the Integrilin to Manage Platelet Aggregation to<br />
prevent Coronary Thrombosis-II (IMPACT-II) trial, a double-blind,<br />
randomized, placebo-controlled multicenter trial<br />
that enrolled 4010 patients undergoing coronary angioplasty<br />
(198). Patients were assigned to treatment with aspirin,<br />
heparin and placebo, aspirin, heparin, and eptifibatide bolus<br />
(135 mcg per kg) followed by a low-dose eptifibatide infufor<br />
the CAPTURE investigators, also reported that among<br />
the 1265 patients with UA enrolled in the CAPTURE trial,<br />
troponin T and CK-MB from 890 patients correlated with<br />
subsequent 6-month adverse cardiac risk. In patients without<br />
elevated troponin T levels, there was no benefit of treatment<br />
with respect to the relative risk of death or MI at 6 months<br />
(OR 1.26, CI 95% 0.74 to 2.31; P equals 0.47). Serum troponin<br />
T level, which is considered to be a surrogate marker<br />
for thrombus formation, identified a high-risk subgroup of<br />
patients with refractory UA suitable for coronary intervention<br />
who would particularly benefit from antiplatelet treatment<br />
with abciximab (192).<br />
One putative limitation of abciximab is the potential for<br />
immune-mediated hypersensitivity reactions after subsequent<br />
readministration. Thrombocytopenia after readministration<br />
occurs in 3.5% to 6.3% of patients, which is similar to<br />
the rate of occurrence in patients receiving abciximab for the<br />
first time. Therefore, the absence of thrombocytopenia after<br />
a first abciximab exposure does not guarantee protection<br />
against its occurrence upon re-exposure. Moreover, the<br />
prevalence of severe thrombocytopenia (2.8%) and profound<br />
thrombocytopenia (2.0%) is greater with readministration<br />
than the incidence observed after first-time administration<br />
(1.0% and 0.4% for severe and profound thrombocytopenia,<br />
respectively) (202). With the first administration, human<br />
antichimeric antibodies (HACA) form in approximately 6%<br />
of patients (702). The implications of HACA, however, are<br />
unclear. Among 500 patients enrolled in the ReoPro<br />
Readministration Registry (R3), there were no cases of anaphylaxis<br />
or other allergic manifestations whether or not<br />
HACA was present, and HACA was not predictive of any<br />
other measure of complication or success. From the R3<br />
study, HACA has been shown to be an IgG (not IgE)<br />
immunoglobulin that does not neutralize abciximab. The<br />
more worrisome clinical phenomenon associated with readministration<br />
is the potential for increased rates of thrombocytopenia.<br />
In the 500-patient R3, a 4.4% incidence in thrombocytopenia<br />
(to a platelet count of less than 100 × 109 per<br />
liter) was observed, with half of the patients developing<br />
acute profound thrombocytopenia (to a platelet count of less<br />
than 20 × 109 per liter). This potential complication should<br />
always be monitored when treating a patient with abciximab<br />
(194-197). Abciximab readministration poses greater risk<br />
within 2 weeks of original abciximab dose.<br />
6.2.2.2. Eptifibatide