BULLETIN
CSQ-Bulletin93
CSQ-Bulletin93
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Page 32 | Bulletin 93 | September 2015<br />
stroke, this would make the point that<br />
the surgical intervention is merely<br />
a single, though significant, event<br />
in a longer-term disease process,<br />
demonstrate the importance of<br />
teamwork and collaboration, and<br />
encourage students to follow patients for<br />
longer than they often do. We would be<br />
interested to know if anyone has tried,<br />
or is planning to try, such an approach.<br />
The specialties of anaesthesia, critical<br />
care and pain medicine are well placed<br />
to facilitate the acquisition of much<br />
of the knowledge and understanding,<br />
and many of the skills and attitudes<br />
that are relevant to the newly qualified<br />
doctor caring for the patient in the<br />
perioperative period. While many of<br />
these ‘competencies’ lie within the<br />
domains that traditionally have been<br />
taught during anaesthetic attachments<br />
(applied physiology, pain pharmacology,<br />
airway management, for example),<br />
the anaesthetist is also well placed<br />
to demonstrate and discuss topics<br />
that have become the ‘unofficial’ but<br />
customary preserve of our specialty,<br />
such as patient safety and human<br />
factors, consent, and treatment<br />
limitation (see Table 1). In addition,<br />
we have much to contribute both to the<br />
teaching programmes in other clinical<br />
specialties and to the wide promotion<br />
of areas which are new priorities for<br />
the NHS (e.g. prevention of chronic<br />
ill-health through pain clinic work<br />
and promotion of the general public<br />
health benefits from the perioperative<br />
encounter), as well as long-standing<br />
professional principles which are<br />
being re-emphasised currently (e.g.<br />
humanitarian care of the vulnerable).<br />
Our view is that we should move away<br />
from identifying ourselves as mere<br />
technicians and highlight the many<br />
non-technical roles we play within the<br />
operating theatre, and the influence we<br />
exert throughout the hospital.<br />
The undergraduate curriculum is<br />
well developed, but not yet finalised.<br />
We would encourage those working<br />
in anaesthesia, critical care and pain<br />
management both to comment on the<br />
curriculum proposals and also to share,<br />
if they would like, examples of how<br />
they are currently delivering any of the<br />
above elements to undergraduates. As<br />
the programme develops we would like<br />
to publicise existing good ideas. Please<br />
contact us via perioperativemedicine@<br />
rcoa.ac.uk.<br />
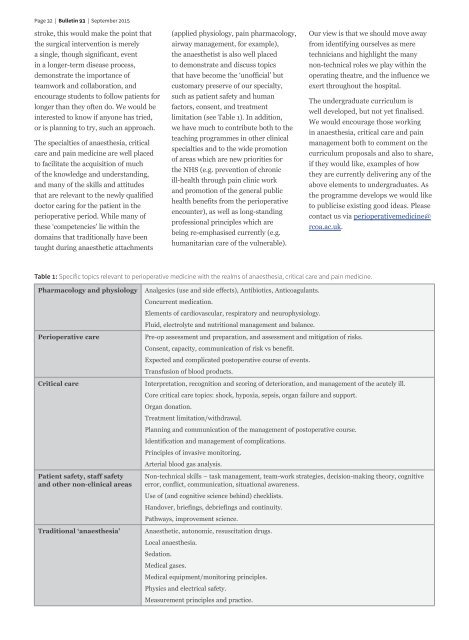
Table 1: Specific topics relevant to perioperative medicine with the realms of anaesthesia, critical care and pain medicine.<br />
Pharmacology and physiology<br />
Perioperative care<br />
Critical care<br />
Patient safety, staff safety<br />
and other non-clinical areas<br />
Traditional ‘anaesthesia’<br />
Analgesics (use and side effects), Antibiotics, Anticoagulants.<br />
Concurrent medication.<br />
Elements of cardiovascular, respiratory and neurophysiology.<br />
Fluid, electrolyte and nutritional management and balance.<br />
Pre-op assessment and preparation, and assessment and mitigation of risks.<br />
Consent, capacity, communication of risk vs benefit.<br />
Expected and complicated postoperative course of events.<br />
Transfusion of blood products.<br />
Interpretation, recognition and scoring of deterioration, and management of the acutely ill.<br />
Core critical care topics: shock, hypoxia, sepsis, organ failure and support.<br />
Organ donation.<br />
Treatment limitation/withdrawal.<br />
Planning and communication of the management of postoperative course.<br />
Identification and management of complications.<br />
Principles of invasive monitoring.<br />
Arterial blood gas analysis.<br />
Non-technical skills – task management, team-work strategies, decision-making theory, cognitive<br />
error, conflict, communication, situational awareness.<br />
Use of (and cognitive science behind) checklists.<br />
Handover, briefings, debriefings and continuity.<br />
Pathways, improvement science.<br />
Anaesthetic, autonomic, resuscitation drugs.<br />
Local anaesthesia.<br />
Sedation.<br />
Medical gases.<br />
Medical equipment/monitoring principles.<br />
Physics and electrical safety.<br />
Measurement principles and practice.