AAHS ASPN ASRM - 2013 Annual Meeting - American Association ...
AAHS ASPN ASRM - 2013 Annual Meeting - American Association ...
AAHS ASPN ASRM - 2013 Annual Meeting - American Association ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Metacarpal and Phalangeal Fractures<br />
Michael S. Bednar, MD<br />
Chief, Section of Hand Surgery<br />
Associate Professor<br />
Dept. of Orthopaedic Surgery and Rehabilitation<br />
Loyola University – Chicago<br />
Introduction<br />
Incidence – metacarpal and phalangeal fractures – 10% of all fractures<br />
Location<br />
Distal phalanx (45-50%)<br />
Metacarpal (30-35%)<br />
Proximal phalanx (15-20%)<br />
Middle phalanx (8-12%)<br />
“Phalangeal fracture of the hand. An analysis of gender and age-related incidence and aetiology.” De Jonge. JHS 19B,<br />
1994.<br />
10-29 y.o. – sports<br />
40-60 y.o. – industrial injures, highest incidence<br />
>70 y.o. – accidental falls<br />
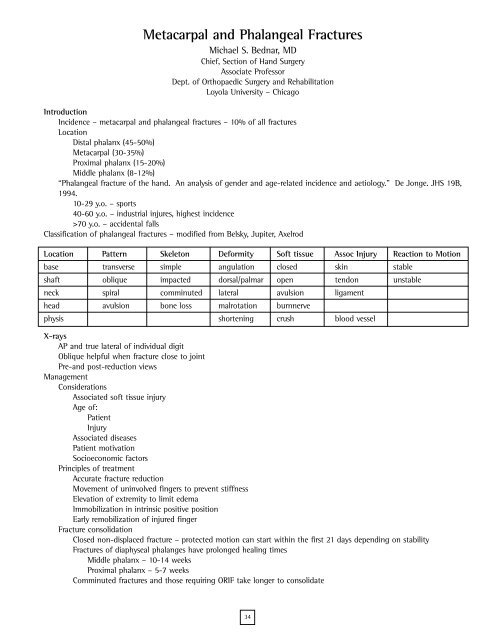
Classification of phalangeal fractures – modified from Belsky, Jupiter, Axelrod<br />
Location Pattern Skeleton Deformity Soft tissue Assoc Injury Reaction to Motion<br />
base transverse simple angulation closed skin stable<br />
shaft oblique impacted dorsal/palmar open tendon unstable<br />
neck spiral comminuted lateral avulsion ligament<br />
head avulsion bone loss malrotation burnnerve<br />
physis shortening crush blood vessel<br />
X-rays<br />
AP and true lateral of individual digit<br />
Oblique helpful when fracture close to joint<br />
Pre-and post-reduction views<br />
Management<br />
Considerations<br />
Associated soft tissue injury<br />
Age of:<br />
Patient<br />
Injury<br />
Associated diseases<br />
Patient motivation<br />
Socioeconomic factors<br />
Principles of treatment<br />
Accurate fracture reduction<br />
Movement of uninvolved fingers to prevent stiffness<br />
Elevation of extremity to limit edema<br />
Immobilization in intrinsic positive position<br />
Early remobilization of injured finger<br />
Fracture consolidation<br />
Closed non-displaced fracture – protected motion can start within the first 21 days depending on stability<br />
Fractures of diaphyseal phalanges have prolonged healing times<br />
Middle phalanx – 10-14 weeks<br />
Proximal phalanx – 5-7 weeks<br />
Comminuted fractures and those requiring ORIF take longer to consolidate<br />
34