Abstraktband als pdf - DGPK-Deutsche Gesellschaft für Pädiatrische ...
Abstraktband als pdf - DGPK-Deutsche Gesellschaft für Pädiatrische ...
Abstraktband als pdf - DGPK-Deutsche Gesellschaft für Pädiatrische ...
Erfolgreiche ePaper selbst erstellen
Machen Sie aus Ihren PDF Publikationen ein blätterbares Flipbook mit unserer einzigartigen Google optimierten e-Paper Software.
44. Jahrestagung der <strong>Deutsche</strong>n <strong>Gesellschaft</strong> für Pädiatrische Kardiologie<br />
– Abstracts –<br />
27<br />
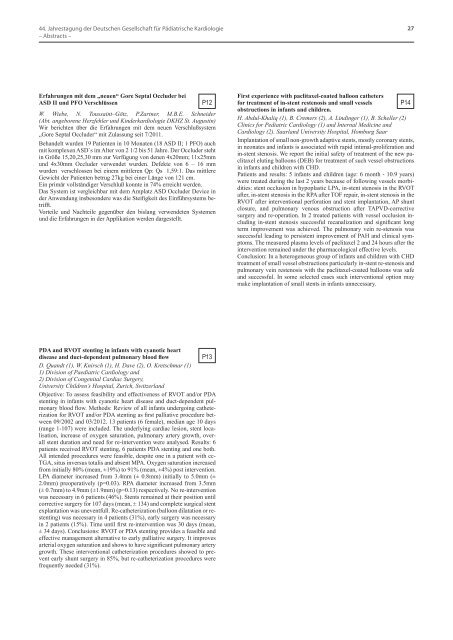
Erfahrungen mit dem „neuen“ Gore Septal Occluder bei<br />
ASD II und PFO Verschlüssen<br />
P12<br />
W. Wiebe, N. Toussaint–Götz, P.Zartner, M.B.E. Schneider<br />
(Abt. angeborene Herzfehler und Kinderkardiologie DKHZ St. Augustin)<br />
Wir berichten über die Erfahrungen mit dem neuen Verschlußsystem<br />
„Gore Septal Occluder“ mit Zulassung seit 7/2011.<br />
Behandelt wurden 19 Patienten in 10 Monaten (18 ASD II; 1 PFO) auch<br />
mit komplexen ASD`s im Alter von 2 1/2 bis 51 Jahre. Der Occluder steht<br />
in Größe 15,20,25,30 mm zur Verfügung von denen 4x20mm; 11x25mm<br />
und 4x30mm Occluder verwendet wurden. Defekte von 6 – 16 mm<br />
wurden verschlossen bei einem mittleren Qp: Qs 1,59:1. Das mittlere<br />
Gewicht der Patienten betrug 27kg bei einer Länge von 121 cm.<br />
Ein primär vollständiger Verschluß konnte in 74% erreicht werden.<br />
Das System ist vergleichbar mit dem Amplatz ASD Occluder Device in<br />
der Anwendung insbesondere was die Steifigkeit des Einführsystems betrifft.<br />
Vorteile und Nachteile gegenüber den bislang verwendeten Systemen<br />
und die Erfahrungen in der Applikation werden dargestellt.<br />
First experience with paclitaxel-coated balloon catheters<br />
for treatment of in-stent restenosis and small vessels P14<br />
obstructions in infants and children.<br />
H. Abdul-Khaliq (1), B. Cremers (2), A. Lindinger (1), B. Scheller (2)<br />
Clinics for Pediatric Cardiology (1) and Internal Medicine and<br />
Cardiology (2). Saarland University Hospital, Homburg Saar<br />
Implantation of small non-growth adaptive stents, mostly coronary stents,<br />
in neonates and infants is associated with rapid intimal-proliferation and<br />
in-stent stenosis. We report the initial safety of treatment of the new paclitaxel<br />
eluting balloons (DEB) for treatment of such vessel obstructions<br />
in infants and children with CHD.<br />
Patients and results: 5 infants and children (age: 6 month - 10.9 years)<br />
were treated during the last 2 years because of following vessels morbidities:<br />
stent occlusion in hypoplastic LPA, in-stent stenosis in the RVOT<br />
after, in-stent stenosis in the RPA after TOF repair, in-stent stenosis in the<br />
RVOT after interventional perforation and stent implantation, AP shunt<br />
closure, and pulmonary venous obstruction after TAPVD-corrective<br />
surgery and re-operation. In 2 treated patients with vessel occlusion including<br />
in-stent stenosis successful recanalization and significant long<br />
term improvement was achieved. The pulmonary vein re-stenosis was<br />
successful leading to persistent improvement of PAH and clinical symptoms.<br />
The measured plasma levels of paclitaxel 2 and 24 hours after the<br />
intervention remained under the pharmacological effective levels.<br />
Conclusion: In a heterogeneous group of infants and children with CHD<br />
treatment of small vessel obstructions particularly in-stent re-stenosis and<br />
pulmonary vein restenosis with the paclitaxel-coated balloons was safe<br />
and successful. In some selected cases such interventional option may<br />
make implantation of small stents in infants unnecessary.<br />
PDA and RVOT stenting in infants with cyanotic heart<br />
disease and duct-dependent pulmonary blood flow P13<br />
D. Quandt (1), W. Knirsch (1), H. Dave (2), O. Kretschmar (1)<br />
1) Division of Paediatric Cardiology and<br />
2) Division of Congenital Cardiac Surgery,<br />
University Children’s Hospital, Zurich, Switzerland<br />
Objective: To assess feasibility and effectiveness of RVOT and/or PDA<br />
stenting in infants with cyanotic heart disease and duct-dependent pulmonary<br />
blood flow. Methods: Review of all infants undergoing catheterization<br />
for RVOT and/or PDA stenting as first palliative procedure between<br />
09/2002 and 03/2012. 13 patients (6 female), median age 10 days<br />
(range 1-107) were included. The underlying cardiac lesion, stent localisation,<br />
increase of oxygen saturation, pulmonary artery growth, overall<br />
stent duration and need for re-intervention were analysed. Results: 6<br />
patients received RVOT stenting, 6 patients PDA stenting and one both.<br />
All intended procedures were feasible, despite one in a patient with cc-<br />
TGA, situs inversus totalis and absent MPA. Oxygen saturation increased<br />
from initially 80% (mean, ±19%) to 91% (mean, ±4%) post intervention.<br />
LPA diameter increased from 3.4mm (± 0.8mm) initially to 5.0mm (±<br />
2.0mm) preoperatively (p=0.03). RPA diameter increased from 3.5mm<br />
(± 0.7mm) to 4.9mm (±1.9mm) (p=0.13) respectively. No re-intervention<br />
was necessary in 6 patients (46%). Stents remained at their position until<br />
corrective surgery for 107 days (mean, ± 134) and complete surgical stent<br />
explantation was uneventfull. Re-catheterization (balloon dilatation or restenting)<br />
was necessary in 4 patients (31%), early surgery was necessary<br />
in 2 patients (15%). Time until first re-intervention was 30 days (mean,<br />
± 34 days). Conclusions: RVOT or PDA stenting provides a feasible and<br />
effective management alternative to early palliative surgery. It improves<br />
arterial oxygen saturation and shows to have significant pulmonary artery<br />
growth. These interventional catheterization procedures showed to prevent<br />
early shunt surgery in 85%, but re-catheterization procedures were<br />
frequently needed (31%).