DM Full Guideline (2010) - VA/DoD Clinical Practice Guidelines Home
DM Full Guideline (2010) - VA/DoD Clinical Practice Guidelines Home
DM Full Guideline (2010) - VA/DoD Clinical Practice Guidelines Home
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Version 4.0<br />
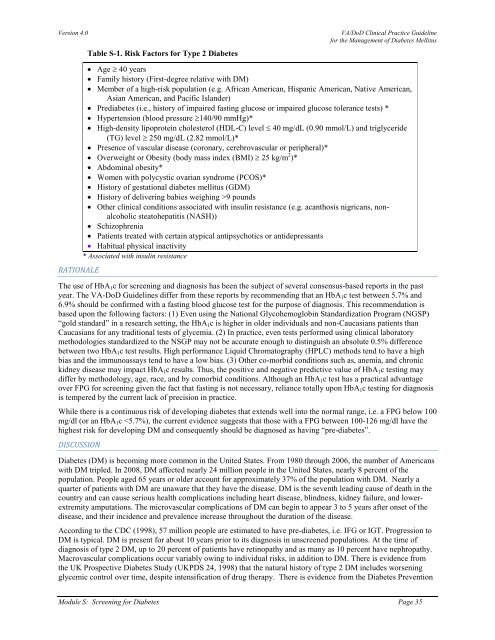
Table S-1. Risk Factors for Type 2 Diabetes<br />
<strong>VA</strong>/<strong>DoD</strong> <strong>Clinical</strong> <strong>Practice</strong> <strong>Guideline</strong><br />
for the Management of Diabetes Mellitus<br />
RATIONALE<br />
• Age ≥ 40 years<br />
• Family history (First-degree relative with <strong>DM</strong>)<br />
• Member of a high-risk population (e.g. African American, Hispanic American, Native American,<br />
Asian American, and Pacific Islander)<br />
• Prediabetes (i.e., history of impaired fasting glucose or impaired glucose tolerance tests) *<br />
• Hypertension (blood pressure ≥140/90 mmHg)*<br />
• High-density lipoprotein cholesterol (HDL-C) level ≤ 40 mg/dL (0.90 mmol/L) and triglyceride<br />
(TG) level ≥ 250 mg/dL (2.82 mmol/L)*<br />
• Presence of vascular disease (coronary, cerebrovascular or peripheral)*<br />
• Overweight or Obesity (body mass index (BMI) ≥ 25 kg/m 2 )*<br />
• Abdominal obesity*<br />
• Women with polycystic ovarian syndrome (PCOS)*<br />
• History of gestational diabetes mellitus (G<strong>DM</strong>)<br />
• History of delivering babies weighing >9 pounds<br />
• Other clinical conditions associated with insulin resistance (e.g. acanthosis nigricans, nonalcoholic<br />
steatohepatitis (NASH))<br />
• Schizophrenia<br />
• Patients treated with certain atypical antipsychotics or antidepressants<br />
• Habitual physical inactivity<br />
* Associated with insulin resistance<br />
The use of HbA 1 c for screening and diagnosis has been the subject of several consensus-based reports in the past<br />
year. The <strong>VA</strong>-<strong>DoD</strong> <strong>Guideline</strong>s differ from these reports by recommending that an HbA 1 c test between 5.7% and<br />
6.9% should be confirmed with a fasting blood glucose test for the purpose of diagnosis. This recommendation is<br />
based upon the following factors: (1) Even using the National Glycohemoglobin Standardization Program (NGSP)<br />
“gold standard” in a research setting, the HbA 1 c is higher in older individuals and non-Caucasians patients than<br />
Caucasians for any traditional tests of glycemia. (2) In practice, even tests performed using clinical laboratory<br />
methodologies standardized to the NSGP may not be accurate enough to distinguish an absolute 0.5% difference<br />
between two HbA 1 c test results. High performance Liquid Chromatography (HPLC) methods tend to have a high<br />
bias and the immunoassays tend to have a low bias. (3) Other co-morbid conditions such as, anemia, and chronic<br />
kidney disease may impact HbA 1 c results. Thus, the positive and negative predictive value of HbA 1 c testing may<br />
differ by methodology, age, race, and by comorbid conditions. Although an HbA 1 c test has a practical advantage<br />
over FPG for screening given the fact that fasting is not necessary, reliance totally upon HbA 1 c testing for diagnosis<br />
is tempered by the current lack of precision in practice.<br />
While there is a continuous risk of developing diabetes that extends well into the normal range, i.e. a FPG below 100<br />
mg/dl (or an HbA 1 c