DM Full Guideline (2010) - VA/DoD Clinical Practice Guidelines Home
DM Full Guideline (2010) - VA/DoD Clinical Practice Guidelines Home
DM Full Guideline (2010) - VA/DoD Clinical Practice Guidelines Home
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Version 4.0<br />
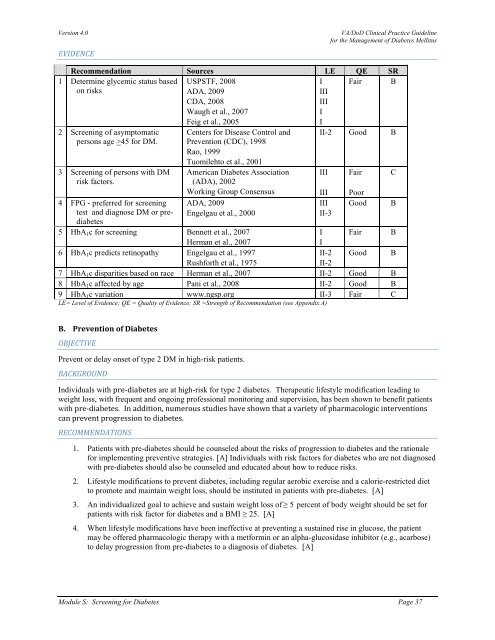
EVIDENCE<br />
<strong>VA</strong>/<strong>DoD</strong> <strong>Clinical</strong> <strong>Practice</strong> <strong>Guideline</strong><br />
for the Management of Diabetes Mellitus<br />
Recommendation Sources LE QE SR<br />
1 Determine glycemic status based<br />
on risks<br />
Fair B<br />
2 Screening of asymptomatic<br />
persons age >45 for <strong>DM</strong>.<br />
3 Screening of persons with <strong>DM</strong><br />
risk factors.<br />
4 FPG - preferred for screening<br />
test and diagnose <strong>DM</strong> or prediabetes<br />
USPSTF, 2008<br />
ADA, 2009<br />
CDA, 2008<br />
Waugh et al., 2007<br />
Feig et al., 2005<br />
Centers for Disease Control and<br />
Prevention (CDC), 1998<br />
Rao, 1999<br />
Tuomilehto et al., 2001<br />
American Diabetes Association<br />
(ADA), 2002<br />
Working Group Consensus<br />
ADA, 2009<br />
Engelgau et al., 2000<br />
I<br />
III<br />
III<br />
I<br />
I<br />
II-2 Good B<br />
III<br />
III<br />
III<br />
II-3<br />
Fair<br />
Poor<br />
Good<br />
5 HbA 1 c for screening Bennett et al., 2007<br />
I Fair B<br />
Herman et al., 2007<br />
I<br />
6 HbA 1 c predicts retinopathy Engelgau et al., 1997<br />
II-2 Good B<br />
Rushforth et al., 1975<br />
II-2<br />
7 HbA 1 c disparities based on race Herman et al., 2007 II-2 Good B<br />
8 HbA 1 c affected by age Pani et al., 2008 II-2 Good B<br />
9 HbA 1 c variation www.ngsp.org II-3 Fair C<br />
LE= Level of Evidence; QE = Quality of Evidence; SR =Strength of Recommendation (see Appendix A)<br />
C<br />
B<br />
B. Prevention of Diabetes<br />
OBJECTIVE<br />
Prevent or delay onset of type 2 <strong>DM</strong> in high-risk patients.<br />
BACKGROUND<br />
Individuals with pre-diabetes are at high-risk for type 2 diabetes. Therapeutic lifestyle modification leading to<br />
weight loss, with frequent and ongoing professional monitoring and supervision, has been shown to benefit patients<br />
with pre-diabetes. In addition, numerous studies have shown that a variety of pharmacologic interventions<br />
can prevent progression to diabetes.<br />
RECOMMENDATIONS<br />
1. Patients with pre-diabetes should be counseled about the risks of progression to diabetes and the rationale<br />
for implementing preventive strategies. [A] Individuals with risk factors for diabetes who are not diagnosed<br />
with pre-diabetes should also be counseled and educated about how to reduce risks.<br />
2. Lifestyle modifications to prevent diabetes, including regular aerobic exercise and a calorie-restricted diet<br />
to promote and maintain weight loss, should be instituted in patients with pre-diabetes. [A]<br />
3. An individualized goal to achieve and sustain weight loss of ≥ 5 percent of body weight should be set for<br />
patients with risk factor for diabetes and a BMI ≥ 25. [A]<br />
4. When lifestyle modifications have been ineffective at preventing a sustained rise in glucose, the patient<br />
may be offered pharmacologic therapy with a metformin or an alpha-glucosidase inhibitor (e.g., acarbose)<br />
to delay progression from pre-diabetes to a diagnosis of diabetes. [A]<br />
Module S: Screening for Diabetes Page 37