Clinical Guidelines for Acute Stroke Management - Living on the EDge
Clinical Guidelines for Acute Stroke Management - Living on the EDge
Clinical Guidelines for Acute Stroke Management - Living on the EDge
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
4 ACUTE MEDICAL & SURGICAL MANAGEMENT<br />
Secti<strong>on</strong> 4 as a whole was given a c<strong>on</strong>sumer rating of 10/10.<br />
Secti<strong>on</strong> 4 <str<strong>on</strong>g>Acute</str<strong>on</strong>g> Medical & Surgical <str<strong>on</strong>g>Management</str<strong>on</strong>g><br />
4.1 Ischaemic stroke and TIA<br />
4.1.1 Early management of TIA<br />
<str<strong>on</strong>g>Management</str<strong>on</strong>g> of TIA involves early risk factor<br />
management to prevent fur<strong>the</strong>r ischaemic events.<br />
An initial policy of commencing aspirin as so<strong>on</strong> as<br />
haemorrhage has been excluded <strong>on</strong> CT or MRI is<br />
recommended early after ischaemic event (see Secti<strong>on</strong><br />
4.1.3). While <strong>the</strong>re is a lower l<strong>on</strong>g term risk of stroke in<br />
those with TIA and AF compared to previous stroke<br />
and AF 118 <strong>the</strong>re is str<strong>on</strong>g evidence <str<strong>on</strong>g>for</str<strong>on</strong>g> <strong>the</strong> l<strong>on</strong>g term<br />
use of anticoagulati<strong>on</strong> in patients with c<strong>on</strong>comitant<br />
AF. 118, 119 O<strong>the</strong>r sec<strong>on</strong>dary preventi<strong>on</strong> management<br />
is <strong>the</strong> same as that outlined <str<strong>on</strong>g>for</str<strong>on</strong>g> those with stroke<br />
(see Secti<strong>on</strong> 7).<br />
4.1.2 Thrombolysis<br />
Two systematic reviews have been undertaken<br />
to determine <strong>the</strong> benefits of thrombolysis in acute<br />
ischaemic stroke. 120, 121 Four different agents have<br />
been evaluated: streptokinase, recombinant<br />
pro-urokinase, recombinant tissue plasminogen<br />
activator (rt-PA) and urokinase. Most of <strong>the</strong> data are<br />
from trials of intravenous thrombolysis involving rt-PA.<br />
Results found:<br />
> Thrombolysis in all trials and all agents combined<br />
results in a significant reducti<strong>on</strong> in <strong>the</strong> composite<br />
end-point of death or disability;<br />
> Thrombolysis (all agents pooled) shows a net<br />
benefit, but is associated with a definite risk of<br />
intracerebral haemorrhage and increased mortality<br />
at <strong>the</strong> end of 3 or 6 m<strong>on</strong>th follow-up.<br />
> Heterogeneity between <strong>the</strong> trials was evident and<br />
no clear evidence <str<strong>on</strong>g>for</str<strong>on</strong>g> <strong>on</strong>e agent, dose or route was<br />
found. There was indirect evidence that rt-PA may<br />
have more benefit and less hazard.<br />
> Therapy appears most beneficial if provided in<br />
experienced centres in highly selected patients.<br />
Widespread use of thrombolytic <strong>the</strong>rapy in routine<br />
clinical practice in n<strong>on</strong> organised stroke care is not<br />
recommended. 120<br />
Subsequent pooled analysis from <strong>the</strong> rt-PA trials<br />
c<strong>on</strong>firm that treatment with intravenous rt-PA has a<br />
clear net benefit in reducing <strong>the</strong> odds of death or<br />
dependency if given within 3 hours. 122 Cases treated<br />
within 3 hours showed 30% greater odds of functi<strong>on</strong>al<br />
independence with a 12% absolute difference<br />
between <strong>the</strong> rt-PA treatment group and placebo<br />
treated patients (number needed to treat of<br />
approximately 8). 122 Treatment given between 3-6<br />
hours from stroke <strong>on</strong>set also appears promising and<br />
fur<strong>the</strong>r trials are underway (e.g. IST-3, ECASS-III).<br />
Subsequent phase IV studies have generally<br />
dem<strong>on</strong>strated similar outcomes to <strong>the</strong> major phase III<br />
studies. 123 Protocol deviati<strong>on</strong> has been identified<br />
across <strong>on</strong>e network of hospitals as a potential reas<strong>on</strong><br />
<str<strong>on</strong>g>for</str<strong>on</strong>g> poorer clinical outcomes in routine practice as<br />
compared to <strong>the</strong> outcomes obtained in <strong>the</strong> treatment<br />
arms of <strong>the</strong> randomised trials. 124 However, an audit<br />
and quality improvement process in <strong>the</strong>se same<br />
hospitals subsequently dem<strong>on</strong>strated a reducti<strong>on</strong> in<br />
protocol violati<strong>on</strong>s (50% down to 19.1% following <strong>the</strong><br />
quality improvement) and an associated decline in<br />
adverse events from 15.7% to 6.4%. 125 Close<br />
m<strong>on</strong>itoring of outcomes, audit and quality<br />
improvement activities are, <strong>the</strong>re<str<strong>on</strong>g>for</str<strong>on</strong>g>e, str<strong>on</strong>gly<br />
recommended <str<strong>on</strong>g>for</str<strong>on</strong>g> all centres delivering rt-PA. The<br />
internati<strong>on</strong>al “Safe Implementati<strong>on</strong> of Thrombolysis<br />
in <str<strong>on</strong>g>Stroke</str<strong>on</strong>g>” (SITS) register is available to support data<br />
collecti<strong>on</strong>, audit and benchmarking across centres<br />
and across countries. Recent safety and clinical<br />
outcome data from <strong>the</strong> European arm of <strong>the</strong> SITS<br />
registry suggests lower adverse events than those<br />
seen in <strong>the</strong> clinical trials of rt-PA. 126 Current Australian<br />
data are comparable to <strong>the</strong> internati<strong>on</strong>al data and are<br />
shown in <strong>the</strong> table below.<br />
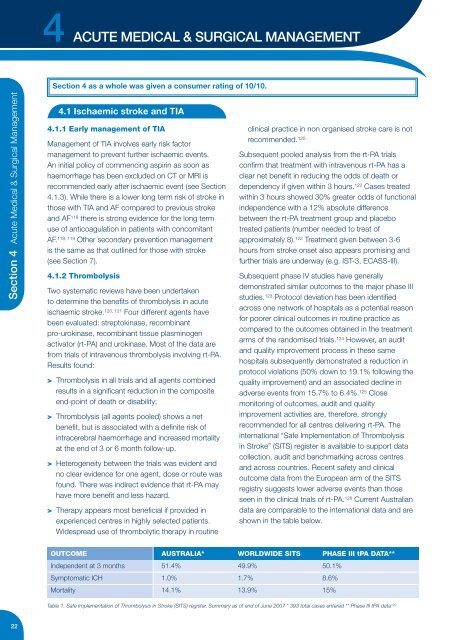
OUTCOME AUSTRALIA* WORLDWIDE SITS PHASE III tPA DATA**<br />
Independent at 3 m<strong>on</strong>ths 51.4% 49.9% 50.1%<br />
Symptomatic ICH 1.0% 1.7% 8.6%<br />
Mortality 14.1% 13.9% 15%<br />
Table 1. Safe Implementati<strong>on</strong> of Thrombolysis in <str<strong>on</strong>g>Stroke</str<strong>on</strong>g> (SITS) register. Summary as of end of June 2007 * 393 total cases entered ** Phase III tPA data 122<br />
22