2008 Summer Meeting - Leeds - The Pathological Society of Great ...
2008 Summer Meeting - Leeds - The Pathological Society of Great ...
2008 Summer Meeting - Leeds - The Pathological Society of Great ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
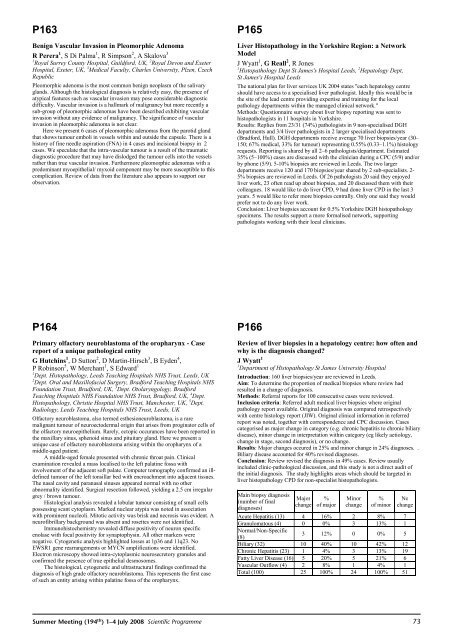
P163Benign Vascular Invasion in Pleomorphic AdenomaR Perera 1 ,SDi Palma 1 , R Simpson 2 , A Skalova 31 Royal Surrey County Hospital, Guildford, UK, 2 Royal Devon and ExeterHospital, Exeter, UK, 3 Medical Faculty, Charles University, Plzen, CzechRepublicPleomorphic adenoma is the most common benign neoplasm <strong>of</strong> the salivaryglands. Although the histological diagnosis is relatively easy, the presence <strong>of</strong>atypical features such as vascular invasion may pose considerable diagnosticdifficulty. Vascular invasion is a hallmark <strong>of</strong> malignancy but more recently asub-group <strong>of</strong> pleomorphic adenomas have been described exhibiting vascularinvasion without any evidence <strong>of</strong> malignancy. <strong>The</strong> significance <strong>of</strong> vascularinvasion in pleomorphic adenoma is not clear.Here we present 6 cases <strong>of</strong> pleomorphic adenomas from the parotid glandthat shows tumour emboli in vessels within and outside the capsule. <strong>The</strong>re is ahistory <strong>of</strong> fine needle aspiration (FNA) in 4 cases and incisional biopsy in 2cases. We speculate that the intra-vascular tumour is a result <strong>of</strong> the traumaticdiagnostic procedure that may have dislodged the tumour cells into the vesselsrather than true vascular invasion. Furthermore pleomorphic adenomas with apredominant myoepithelial/ myxoid component may be more susceptible to thiscomplication. Review <strong>of</strong> data from the literature also appears to support ourobservation.P165Liver Histopathology in the Yorkshire Region: a NetworkModelJWyatt 1 , G Reall 2 ,RJones1 Histopathology Dept St James's Hospital <strong>Leeds</strong>, 2 Hepatology Dept,St James's Hospital <strong>Leeds</strong><strong>The</strong> national plan for liver services UK 2004 states "each hepatology centreshould have access to a specialised liver pathologist. Ideally this would be inthe site <strong>of</strong> the lead centre providing expertise and training for the localpathology departments within the managed clinical network."Methods: Questionnaire survey about liver biopsy reporting was sent tohistopathologists in 11 hospitals in Yorkshire.Results: Replies from 23/31 (74%) pathologists in 9 non-specialised DGHdepartments and 3/4 liver pathologists in 2 larger specialised departments(Bradford, Hull). DGH departments receive average 70 liver biopsies/year (30–150; 67% medical, 33% for tumour) representing 0.55% (0.33–1.1%) histologyrequests. Reporting is shared by all 2–6 pathologists/department. Estimated35% (5–100%) cases are discussed with the clinician during a CPC (5/9) and/orby phone (5/9). 5-10% biopsies are reviewed in <strong>Leeds</strong>. <strong>The</strong> two largerdepartments receive 120 and 170 biopsies/year shared by 2 sub-specialists. 2-5% biopsies are reviewed in <strong>Leeds</strong>. Of 26 pathologists 20 said they enjoyedliver work, 23 <strong>of</strong>ten read up about biopsies, and 20 discussed them with theircolleagues. 18 would like to do liver CPD, 9 had done liver CPD in the last 3years. 5 would like to refer more biopsies centrally. Only one said they wouldprefer not to do any liver work.Conclusion: Liver biopsies account for 0.5% Yorkshire DGH histopathologyspecimens. <strong>The</strong> results support a more formalised network, supportingpathologists working with their local clinicians.P164Primary olfactory neuroblastoma <strong>of</strong> the oropharynx - Casereport <strong>of</strong> a unique pathological entityG Hutchins 1 , D Sutton 2 , D Martin-Hirsch 3 ,BEyden 4 ,P Robinson 5 , W Merchant 1 ,SEdward 11 Dept. Histopathology, <strong>Leeds</strong> Teaching Hospitals NHS Trust, <strong>Leeds</strong>, UK2 Dept. Oral and Maxill<strong>of</strong>acial Surgery, Bradford Teaching Hospitals NHSFoundation Trust, Bradford, UK, 3 Dept. Otolaryngology, BradfordTeaching Hosptials NHS Foundation NHS Trust, Bradford, UK, 4 Dept.Histopathology, Christie Hospital NHS Trust, Manchester, UK, 5 Dept.Radiology, <strong>Leeds</strong> Teaching Hospitals NHS Trust, <strong>Leeds</strong>, UKOlfactory neuroblastoma, also termed esthesioneuroblastoma, is a raremalignant tumour <strong>of</strong> neuroectodermal origin that arises from proginator cells <strong>of</strong>the olfactory neuroepithelium. Rarely, ectopic occurances have been reported inthe maxillary sinus, sphenoid sinus and pituitary gland. Here we present aunique case <strong>of</strong> olfactory neuroblastoma arising within the oropharynx <strong>of</strong> amiddle-aged patient.A middle-aged female presented with chronic throat pain. Clinicalexamination revealed a mass localised to the left palatine fossa withinvolvement <strong>of</strong> the adjacent s<strong>of</strong>t palate. Computer tomography confirmed an illdefinedtumour <strong>of</strong> the left tonsillar bed with encroachment into adjacent tissues.<strong>The</strong> nasal cavity and paranasal sinuses appeared normal with no otherabnormality identified. Surgical resection followed, yielding a 2.5 cm irregulargrey / brown tumour.Histological analysis revealed a lobular tumour consisting <strong>of</strong> small cellspossessing scant cytoplasm. Marked nuclear atypia was noted in associationwith prominent nucleoli. Mitotic activity was brisk and necrosis was evident. Aneur<strong>of</strong>ibrillary background was absent and rosettes were not identified.Immunohistochemistry revealed diffuse positivity <strong>of</strong> neuron specificenolase with focal positivity for synaptophysin. All other markers werenegative. Cytogenetic analysis highlighted losses at 1p36 and 11q23. NoEWSR1 gene rearrangements or MYCN amplifications were identified.Electron microscopy showed intra-cytoplasmic neurosecretory granules andconfirmed the presence <strong>of</strong> true epithelial desmosomes.<strong>The</strong> histological, cytogenetic and ultrastructural findings confirmed thediagnosis <strong>of</strong> high grade olfactory neuroblastoma. This represents the first case<strong>of</strong> such an entity arising within palatine fossa <strong>of</strong> the oropharynx.P166Review <strong>of</strong> liver biopsies in a hepatology centre: how <strong>of</strong>ten andwhy is the diagnosis changed?JWyatt 11 Department <strong>of</strong> Histopathology St James University HospitalIntroduction: 160 liver biopsies/year are reviewed in <strong>Leeds</strong>.Aim: To determine the proportion <strong>of</strong> medical biopsies where review hadresulted in a change <strong>of</strong> diagnosis.Methods: Referral reports for 100 consecutive cases were reviewed.Inclusion criteria: Referred adult medical liver biopsies where originalpathology report available. Original diagnosis was compared retrospectivelywith centre histology report (JIW). Original clinical information in referredreport was noted, together with correspondence and CPC discussion. Casescategorised as major change in category (e.g. chronic hepatitis to chronic biliarydisease), minor change in interpretation within category (eg likely aetiology,change in stage, second diagnosis), or no change.Results: Major changes occured in 25% and minor change in 24% diagnoses. .Biliary disease accounted for 40% revised diagnoses.Conclusion: Review revised the diagnosis in 49% cases. Review usuallyincluded clinic-pathological discussion, and this study is not a direct audit <strong>of</strong>the initial diagnosis. <strong>The</strong> study highlights areas which should be targeted inliver histopathology CPD for non-specialist histopathologists.Main biopsy diagnosis(number <strong>of</strong> finaldiagnoses)Majorchange%<strong>of</strong> majorMinorchange%<strong>of</strong> minorNochangeAcute Hepatitis (13) 4 16% 2 8% 7Granulomatous (4) 0 0% 3 13% 1Normal/Non-Specific(8)3 12% 0 0% 5Biliary (32) 10 40% 10 42% 12Chronic Hepatitis (23) 1 4% 3 13% 19Fatty Liver Disease (16) 5 20% 5 21% 6Vascular Outflow (4) 2 8% 1 4% 1Total (100) 25 100% 24 100% 51<strong>Summer</strong> <strong>Meeting</strong> (194 th ) 1–4 July <strong>2008</strong> Scientific Programme73