EUROHEALTH
Eurohealth-volume22-number2-2016
Eurohealth-volume22-number2-2016
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Moving towards universal health coverage<br />
19<br />
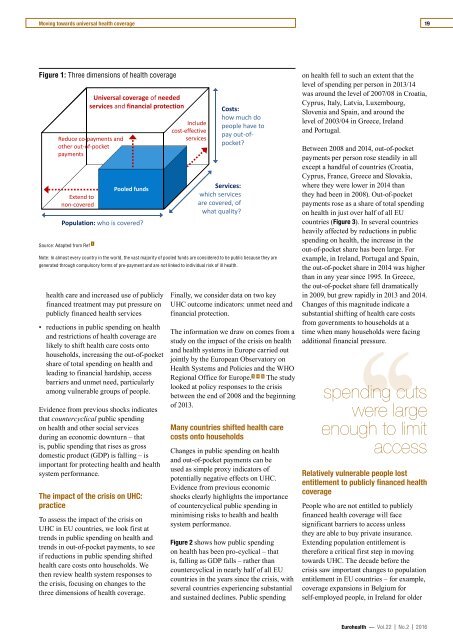
Figure 1: Three dimensions of health coverage<br />
Source: Adapted from Ref 1<br />
Universal coverage of needed<br />
services and financial protection<br />
Reduce co‐payments and<br />
other out‐of‐pocket<br />
payments<br />
Extend to<br />
non‐covered<br />
Pooled funds<br />
Population: who is covered?<br />
health care and increased use of publicly<br />
financed treatment may put pressure on<br />
publicly financed health services<br />
• reductions in public spending on health<br />
and restrictions of health coverage are<br />
likely to shift health care costs onto<br />
households, increasing the out-of-pocket<br />
share of total spending on health and<br />
leading to financial hardship, access<br />
barriers and unmet need, particularly<br />
among vulnerable groups of people.<br />
Evidence from previous shocks indicates<br />
that countercyclical public spending<br />
on health and other social services<br />
during an economic downturn – that<br />
is, public spending that rises as gross<br />
domestic product (GDP) is falling – is<br />
important for protecting health and health<br />
system performance.<br />
The impact of the crisis on UHC:<br />
practice<br />
To assess the impact of the crisis on<br />
UHC in EU countries, we look first at<br />
trends in public spending on health and<br />
trends in out-of-pocket payments, to see<br />
if reductions in public spending shifted<br />
health care costs onto households. We<br />
then review health system responses to<br />
the crisis, focusing on changes to the<br />
three dimensions of health coverage.<br />
Include<br />
cost‐effective<br />
services<br />
Services:<br />
which services<br />
are covered, of<br />
what quality?<br />
Costs:<br />
how much do<br />
people have to<br />
pay out‐ofpocket?<br />
Note: In almost every country in the world, the vast majority of pooled funds are considered to be public because they are<br />
generated through compulsory forms of pre-payment and are not linked to individual risk of ill health.<br />
Finally, we consider data on two key<br />
UHC outcome indicators: unmet need and<br />
financial protection.<br />
The information we draw on comes from a<br />
study on the impact of the crisis on health<br />
and health systems in Europe carried out<br />
jointly by the European Observatory on<br />
Health Systems and Policies and the WHO<br />
Regional Office for Europe. 3 4 5 The study<br />
looked at policy responses to the crisis<br />
between the end of 2008 and the beginning<br />
of 2013.<br />
Many countries shifted health care<br />
costs onto households<br />
Changes in public spending on health<br />
and out-of-pocket payments can be<br />
used as simple proxy indicators of<br />
potentially negative effects on UHC.<br />
Evidence from previous economic<br />
shocks clearly highlights the importance<br />
of countercyclical public spending in<br />
minimising risks to health and health<br />
system performance.<br />
Figure 2 shows how public spending<br />
on health has been pro-cyclical – that<br />
is, falling as GDP falls – rather than<br />
countercyclical in nearly half of all EU<br />
countries in the years since the crisis, with<br />
several countries experiencing substantial<br />
and sustained declines. Public spending<br />
on health fell to such an extent that the<br />
level of spending per person in 2013/14<br />
was around the level of 2007/08 in Croatia,<br />
Cyprus, Italy, Latvia, Luxembourg,<br />
Slovenia and Spain, and around the<br />
level of 2003/04 in Greece, Ireland<br />
and Portugal.<br />
Between 2008 and 2014, out-of-pocket<br />
payments per person rose steadily in all<br />
except a handful of countries (Croatia,<br />
Cyprus, France, Greece and Slovakia,<br />
where they were lower in 2014 than<br />
they had been in 2008). Out-of-pocket<br />
payments rose as a share of total spending<br />
on health in just over half of all EU<br />
countries (Figure 3). In several countries<br />
heavily affected by reductions in public<br />
spending on health, the increase in the<br />
out-of-pocket share has been large. For<br />
example, in Ireland, Portugal and Spain,<br />
the out-of-pocket share in 2014 was higher<br />
than in any year since 1995. In Greece,<br />
the out-of-pocket share fell dramatically<br />
in 2009, but grew rapidly in 2013 and 2014.<br />
Changes of this magnitude indicate a<br />
substantial shifting of health care costs<br />
from governments to households at a<br />
time when many households were facing<br />
‘‘<br />
additional financial pressure.<br />
spending cuts<br />
were large<br />
enough to limit<br />
access<br />
Relatively vulnerable people lost<br />
entitlement to publicly financed health<br />
coverage<br />
People who are not entitled to publicly<br />
financed health coverage will face<br />
significant barriers to access unless<br />
they are able to buy private insurance.<br />
Extending population entitlement is<br />
therefore a critical first step in moving<br />
towards UHC. The decade before the<br />
crisis saw important changes to population<br />
entitlement in EU countries – for example,<br />
coverage expansions in Belgium for<br />
self-employed people, in Ireland for older<br />
Eurohealth — Vol.22 | No.2 | 2016