EUROHEALTH
Eurohealth-volume22-number2-2016
Eurohealth-volume22-number2-2016
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Moving towards universal health coverage<br />
21<br />
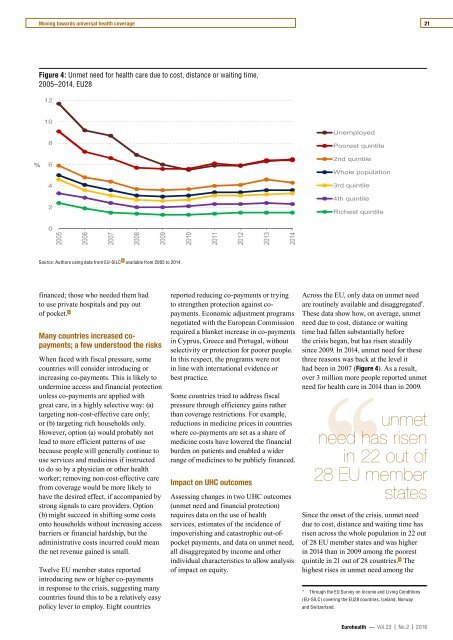
Figure 4: Unmet need for health care due to cost, distance or waiting time,<br />
2005 – 2014, EU28<br />
12<br />
10<br />
%<br />
8<br />
6<br />
4<br />
2<br />
Unemployed<br />
Poorest quintile<br />
2nd quintile<br />
Whole population<br />
3rd quintile<br />
4th quintile<br />
Richest quintile<br />
0<br />
2005<br />
2006<br />
2007<br />
2008<br />
2009<br />
2010<br />
2011<br />
2012<br />
2013<br />
2014<br />
Source: Authors using data from EU-SILC 9 available from 2005 to 2014.<br />
financed; those who needed them had<br />
to use private hospitals and pay out<br />
of pocket. 5<br />
Many countries increased copayments;<br />
a few understood the risks<br />
When faced with fiscal pressure, some<br />
countries will consider introducing or<br />
increasing co-payments. This is likely to<br />
undermine access and financial protection<br />
unless co-payments are applied with<br />
great care, in a highly selective way: (a)<br />
targeting non-cost-effective care only;<br />
or (b) targeting rich households only.<br />
However, option (a) would probably not<br />
lead to more efficient patterns of use<br />
because people will generally continue to<br />
use services and medicines if instructed<br />
to do so by a physician or other health<br />
worker; removing non-cost-effective care<br />
from coverage would be more likely to<br />
have the desired effect, if accompanied by<br />
strong signals to care providers. Option<br />
(b) might succeed in shifting some costs<br />
onto households without increasing access<br />
barriers or financial hardship, but the<br />
administrative costs incurred could mean<br />
the net revenue gained is small.<br />
Twelve EU member states reported<br />
introducing new or higher co-payments<br />
in response to the crisis, suggesting many<br />
countries found this to be a relatively easy<br />
policy lever to employ. Eight countries<br />
reported reducing co-payments or trying<br />
to strengthen protection against copayments.<br />
Economic adjustment programs<br />
negotiated with the European Commission<br />
required a blanket increase in co-payments<br />
in Cyprus, Greece and Portugal, without<br />
selectivity or protection for poorer people.<br />
In this respect, the programs were not<br />
in line with international evidence or<br />
best practice.<br />
Some countries tried to address fiscal<br />
pressure through efficiency gains rather<br />
than coverage restrictions. For example,<br />
reductions in medicine prices in countries<br />
where co-payments are set as a share of<br />
medicine costs have lowered the financial<br />
burden on patients and enabled a wider<br />
range of medicines to be publicly financed.<br />
Impact on UHC outcomes<br />
Assessing changes in two UHC outcomes<br />
(unmet need and financial protection)<br />
requires data on the use of health<br />
services, estimates of the incidence of<br />
impoverishing and catastrophic out-ofpocket<br />
payments, and data on unmet need,<br />
all disaggregated by income and other<br />
individual characteristics to allow analysis<br />
of impact on equity.<br />
Across the EU, only data on unmet need<br />
are routinely available and disaggregated * .<br />
These data show how, on average, unmet<br />
need due to cost, distance or waiting<br />
time had fallen substantially before<br />
the crisis began, but has risen steadily<br />
since 2009. In 2014, unmet need for these<br />
three reasons was back at the level it<br />
had been in 2007 (Figure 4). As a result,<br />
over 3 million more people reported unmet<br />
need for health care in 2014 than in 2009.<br />
need has risen<br />
in 22 out of<br />
28 EU member<br />
‘‘unmet<br />
states<br />
Since the onset of the crisis, unmet need<br />
due to cost, distance and waiting time has<br />
risen across the whole population in 22 out<br />
of 28 EU member states and was higher<br />
in 2014 than in 2009 among the poorest<br />
quintile in 21 out of 28 countries. 9 The<br />
highest rises in unmet need among the<br />
* Through the EU Survey on Income and Living Conditions<br />
(EU-SILC) covering the EU28 countries, Iceland, Norway<br />
and Switzerland.<br />
Eurohealth — Vol.22 | No.2 | 2016