VIable
HLCCompendium
HLCCompendium
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
NDHI<br />
NAT IONAL DIALOGUE FOR<br />
Healthcare Innovation<br />
Coding Advisor<br />
Organization Overview<br />
• Change Healthcare is committed to connecting the<br />
dots between payers, providers, and patients, by<br />
using data analytics to deliver predictive insights<br />
to these clients<br />
• Change Healthcare operates the single largest<br />
financial and administrative healthcare network in<br />
the United States<br />
• The company offers a diverse portfolio of solutions<br />
to help payers, providers, and pharmacies operate<br />
efficiently and effectively<br />
Background<br />
Care practitioners are reimbursed for assessing and<br />
managing patients’ health through a set of Current<br />
Procedural Terminology (CPT) codes called “evaluation<br />
and management” (E/M). These services represent<br />
a significant portion of healthcare billing – 30%<br />
of Medicare Part B payments were for E/M codes in<br />
2010. Improper coding for E/M services is a significant<br />
concern for payers and puts undue financial burden<br />
on the broader healthcare system. The extent of E/M<br />
misuse has been the subject of a report published by<br />
the Office of Inspector General, which found that:<br />
• Medicare paid $6.7 billion in inappropriate E/M<br />
claims in 2010 alone<br />
Traditionally, insurers often pay out claims before<br />
investigating them, due to the short time frames that are<br />
legally-required for provider reimbursement, and then<br />
conduct post-payment audits. When improper coding<br />
occurs, this causes payers to engage in a “pay and<br />
chase” model to adjust reimbursement appropriately to<br />
providers. Due to the high cost in pursuing low dollar,<br />
high-volume claims, payers have historically been unable<br />
to effectively pursue these types of overpayments.<br />
Product Details<br />
Coding Advisor is an innovative platform developed<br />
by Change Healthcare to transform payment integrity<br />
services for the healthcare payer industry. This product<br />
was developed to address the widespread issue of<br />
overpayment by insurers due to:<br />
• Outlier physician E/M upcoding<br />
• Misuse of “modifier 25” for E/M coding<br />
• Unit errors associated with high cost injectable<br />
“J-Code” billings<br />
• 55% of Medicare claims for E/M services were<br />
incorrectly coded or lacking documentation in 2010<br />
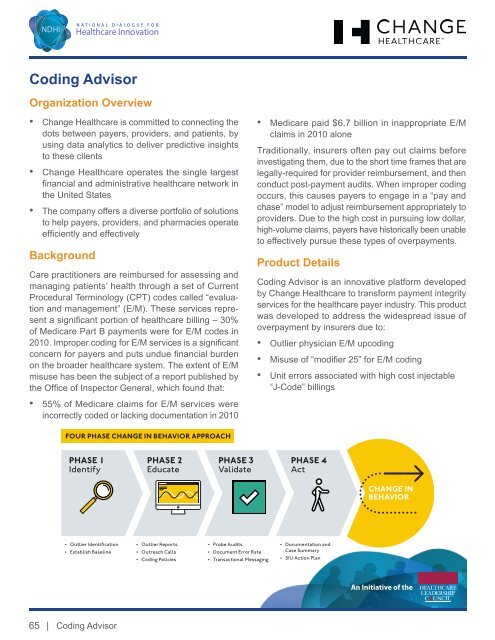
FOUR PHASE CHANGE IN BEHAVIOR APPROACH<br />
PHASE 1<br />
Identify<br />
PHASE 2<br />
Educate<br />
PHASE 3<br />
Validate<br />
PHASE 4<br />
Act<br />
CHANGE IN<br />
BEHAVIOR<br />
• Outlier Identification<br />
• Establish Baseline<br />
• Outlier Reports<br />
• Outreach Calls<br />
• Coding Policies<br />
• Probe Audits<br />
• Document Error Rate<br />
• Transactional Messaging<br />
• Documentation and<br />
Case Summary<br />
• SIU Action Plan<br />
An Initiative of the<br />
65 |<br />
Coding Advisor