Sports Medicine Handbook - NCAA
Sports Medicine Handbook - NCAA
Sports Medicine Handbook - NCAA
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
66<br />
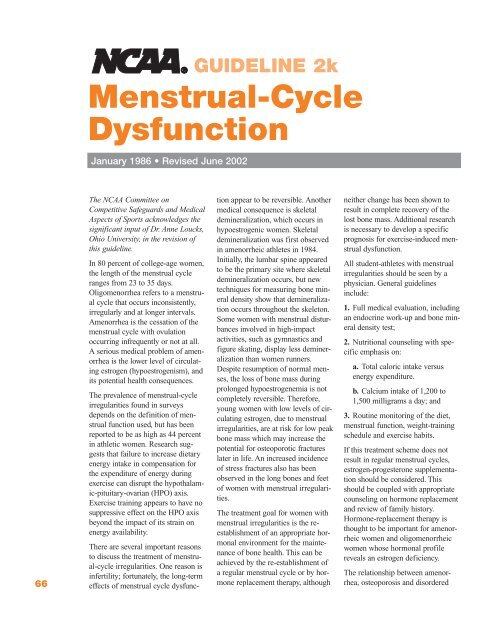
Menstrual-Cycle<br />
Dysfunction<br />
January 1986 • Revised June 2002<br />
The <strong>NCAA</strong> Committee on<br />
Competitive Safeguards and Medical<br />
Aspects of <strong>Sports</strong> acknowledges the<br />
significant input of Dr. Anne Loucks,<br />
Ohio University, in the revision of<br />
this guideline.<br />
In 80 percent of college-age women,<br />
the length of the menstrual cycle<br />
ranges from 23 to 35 days.<br />
Oligomenorrhea refers to a menstrual<br />
cycle that occurs inconsistently,<br />
irregularly and at longer intervals.<br />
Amenorrhea is the cessation of the<br />
menstrual cycle with ovulation<br />
occurring infrequently or not at all.<br />
A serious medical problem of amenorrhea<br />
is the lower level of circulating<br />
estrogen (hypoestrogenism), and<br />
its potential health consequences.<br />
The prevalence of menstrual-cycle<br />
irregularities found in surveys<br />
depends on the definition of menstrual<br />
function used, but has been<br />
reported to be as high as 44 percent<br />
in athletic women. Research suggests<br />
that failure to increase dietary<br />
energy intake in compensation for<br />
the expenditure of energy during<br />
exercise can disrupt the hypothalamic-pituitary-ovarian<br />
(HPO) axis.<br />
Exercise training appears to have no<br />
suppressive effect on the HPO axis<br />
beyond the impact of its strain on<br />
energy availability.<br />
There are several important reasons<br />
to discuss the treatment of menstrual-cycle<br />
irregularities. One reason is<br />
infertility; fortunately, the long-term<br />
effects of menstrual cycle dysfunc-<br />
GUIDELINE 2k<br />
tion appear to be reversible. Another<br />
medical consequence is skeletal<br />
demineralization, which occurs in<br />
hypoestrogenic women. Skeletal<br />
demineralization was first observed<br />
in amenorrheic athletes in 1984.<br />
Initially, the lumbar spine appeared<br />
to be the primary site where skeletal<br />
demineralization occurs, but new<br />
techniques for measuring bone mineral<br />
density show that demineralization<br />
occurs throughout the skeleton.<br />
Some women with menstrual disturbances<br />
involved in high-impact<br />
activities, such as gymnastics and<br />
figure skating, display less demineralization<br />
than women runners.<br />
Despite resumption of normal menses,<br />
the loss of bone mass during<br />
prolonged hypoestrogenemia is not<br />
completely reversible. Therefore,<br />
young women with low levels of circulating<br />
estrogen, due to menstrual<br />
irregularities, are at risk for low peak<br />
bone mass which may increase the<br />
potential for osteoporotic fractures<br />
later in life. An increased incidence<br />
of stress fractures also has been<br />
observed in the long bones and feet<br />
of women with menstrual irregularities.<br />
The treatment goal for women with<br />
menstrual irregularities is the reestablishment<br />
of an appropriate hormonal<br />
environment for the maintenance<br />
of bone health. This can be<br />
achieved by the re-establishment of<br />
a regular menstrual cycle or by hormone<br />
replacement therapy, although<br />
neither change has been shown to<br />
result in complete recovery of the<br />
lost bone mass. Additional research<br />
is necessary to develop a specific<br />
prognosis for exercise-induced menstrual<br />
dysfunction.<br />
All student-athletes with menstrual<br />
irregularities should be seen by a<br />
physician. General guidelines<br />
include:<br />
1. Full medical evaluation, including<br />
an endocrine work-up and bone mineral<br />
density test;<br />
2. Nutritional counseling with specific<br />
emphasis on:<br />
a. Total caloric intake versus<br />
energy expenditure.<br />
b. Calcium intake of 1,200 to<br />
1,500 milligrams a day; and<br />
3. Routine monitoring of the diet,<br />
menstrual function, weight-training<br />
schedule and exercise habits.<br />
If this treatment scheme does not<br />
result in regular menstrual cycles,<br />
estrogen-progesterone supplementation<br />
should be considered. This<br />
should be coupled with appropriate<br />
counseling on hormone replacement<br />
and review of family history.<br />
Hormone-replacement therapy is<br />
thought to be important for amenorrheic<br />
women and oligomenorrheic<br />
women whose hormonal profile<br />
reveals an estrogen deficiency.<br />
The relationship between amenorrhea,<br />
osteoporosis and disordered