Pragmatische Lösung eines komplexen Problems Schweizer ...
Pragmatische Lösung eines komplexen Problems Schweizer ...
Pragmatische Lösung eines komplexen Problems Schweizer ...
Erfolgreiche ePaper selbst erstellen
Machen Sie aus Ihren PDF Publikationen ein blätterbares Flipbook mit unserer einzigartigen Google optimierten e-Paper Software.
Der seltene Fall<br />
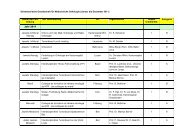
but two endoluminal vegetations were found in the gastric<br />
antrum (with a diameter of about 2.5 cm) and a larger<br />
one (with a diameter of about 3.5 cm) in the proximal<br />
jejunum [Figure 1 and 2]. Endoscopic biopsy of both lesions<br />
was taken. The histological exam of the gastric one<br />
showed a fused cells tumor with a very low proliferation<br />
index and without invasion of the mucosa. The immunohistochemical<br />
profile was positive for S-100 and negative<br />
for CD34 and CD117 and the diagnosis of a mesenchymal<br />
tumor, compatible with a schwannoma, was established.<br />
The jejunum lesion also did not show invasion of the<br />
mucosa, and was constituted of a uniform population of<br />
spindle-shaped cells with a focal extension under the mesothelial<br />
lamina of the visceral peritoneum. The immunohistochemical<br />
panel was negative for S-100 and positive<br />
for CD34 and CD117, the proliferation index was very<br />
low, and the diagnosis of a mesenchymal tumor, compatible<br />
with a gastrointestinal stromal tumor (GIST), was<br />
established. These diagnoses, suggestive for two distinct<br />
neoplastic processes, were later confirmed after a Billroth<br />
II gastrectomy with Roux-en-Y anastomosis and a segmental<br />
jejunal resection in November 2009. The resected<br />
regional lymph nodes resulted negative for neoplastic tissue.<br />
The postoperative course was uncomplicated and the<br />
patient was dismissed.<br />
Before surgery, PET-CT scans showed a moderate positivity<br />
for the two known lesions, but no other suspicious lesions.<br />
In a follow-up CT scan in June 2010, there was no<br />
evidence of relapse.<br />
Discussion<br />
We describe the rare case of a patient who developed concomitantly<br />
a gastric schwannoma and a duodenal GIST 26<br />
years after the first diagnosis of acute promyelocytic leukemia<br />
(APL) repeatedly treated with aggressive chemotherapy<br />
for several relapses and with maintenance therapy<br />
with ATRA protracted for about 12 years.<br />
Acute myeloblastic leukemia (AML) in European adults<br />
represents 5–8 cases per 100 000 yearly and the mortality<br />
figures 4–6 cases per 100 000. A relatively rare subtype<br />
of acute myeloid leukemia is APL, which comprises<br />
about 6%-10% of all AMLs with distinctive morphology<br />
and clinical presentation with coagulopathy [1]. It was<br />
termed M3 in the French–American–British (FAB) criteria<br />
established in 1976 and based on morphology and immunophenotyping.<br />
Nowadays, this disease entity is more<br />
precisely defined by the presence of the t(15;17) (q22;q12)<br />
chromosomal translocation affecting the retinoic acid receptor<br />
alpha gene (RARα) [2].<br />
Acute promyelocytic leukemia was first described in 1957<br />
[3]. During the 1950s through 1970s APL had a 100%<br />
mortality rate primarily due to severe hypofibrinogenopenia<br />
as a result of primary fibrinolysis and disseminated<br />
intravascular coagulation which frequently caused intracerebral<br />
hemorrhage. After the introduction of daunorubicin-based<br />
chemotherapy regimens, the induction of complete<br />
remissions in about the majority of the APL cases<br />
became possible, with a median duration of remission of<br />
more than 2 years [4, 5].<br />
Further treatment progress followed the demonstration<br />
that retinoic acid induces terminal granulocytic differentiation<br />
of human promyelocytic leukemia cells [6] and<br />
that the abnormal accumulation of immature promyelocytes<br />
in APL is linked to chromosomal aberrations involving<br />
the retinoic acid receptor alpha gene. In the late 1980s<br />
it was discovered that the consistent chromosomal aberrations<br />
of APL, t(15;17) (q22;q12) [7], fuses the RARα<br />
gene on chromosome 17 to the promyelocytic leukemia<br />
(PML) gene on chromosome 15, generating the fusion<br />
protein PML-RAR [8-11].<br />
This genetic alteration renders the neoplastic cells particularly<br />
sensitive to ATRA, which induces differentiation<br />
of the leukemic cells into mature granulocytes. The<br />
incorporation of ATRA in induction therapy represented<br />
indeed an important progress in APL, which decreased<br />
the risk of early hemorrhagic complications and death<br />
and enhanced the long term response rate and survival<br />
[12, 13]. APL has nowadays become the most curable<br />
AML subtype in adults and the role of ATRA in its<br />
treatment is considered a paradigm of targeted therapy.<br />
ATRA with anthracycline-based chemotherapy for induction<br />
and consolidation followed by ATRA plus lowdose<br />
chemotherapy maintenance is the current standard<br />
for newly diagnosed patients [14].<br />
Stromal or mesenchymal neoplasms affecting the gastrointestinal<br />
(GI) tract constitute