Contents Chapter Topic Page Neonatology Respiratory Cardiology
Contents Chapter Topic Page Neonatology Respiratory Cardiology
Contents Chapter Topic Page Neonatology Respiratory Cardiology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
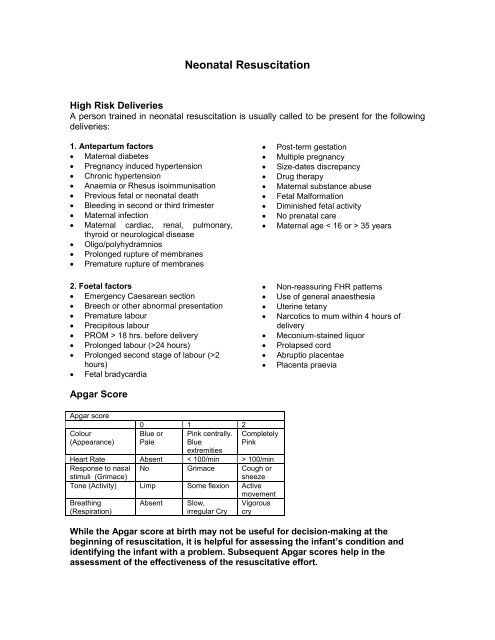
Neonatal Resuscitation<br />
High Risk Deliveries<br />
A person trained in neonatal resuscitation is usually called to be present for the following<br />
deliveries:<br />
1. Antepartum factors<br />
• Maternal diabetes<br />
• Pregnancy induced hypertension<br />
• Chronic hypertension<br />
• Anaemia or Rhesus isoimmunisation<br />
• Previous fetal or neonatal death<br />
• Bleeding in second or third trimester<br />
• Maternal infection<br />
• Maternal cardiac, renal, pulmonary,<br />
thyroid or neurological disease<br />
• Oligo/polyhydramnios<br />
• Prolonged rupture of membranes<br />
• Premature rupture of membranes<br />
2. Foetal factors<br />
• Emergency Caesarean section<br />
• Breech or other abnormal presentation<br />
• Premature labour<br />
• Precipitous labour<br />
• PROM > 18 hrs. before delivery<br />
• Prolonged labour (>24 hours)<br />
• Prolonged second stage of labour (>2<br />
hours)<br />
• Fetal bradycardia<br />
Apgar Score<br />
Apgar score<br />
Colour<br />
(Appearance)<br />
0 1 2<br />
Blue or<br />
Pale<br />
Pink centrally.<br />
Blue<br />
extremities<br />
Completely<br />
Pink<br />
Heart Rate Absent < 100/min > 100/min<br />
Response to nasal No Grimace Cough or<br />
stimuli (Grimace)<br />
sneeze<br />
Tone (Activity) Limp Some flexion Active<br />
movement<br />
Breathing<br />
Absent Slow,<br />
Vigorous<br />
(Respiration)<br />
irregular Cry cry<br />
• Post-term gestation<br />
• Multiple pregnancy<br />
• Size-dates discrepancy<br />
• Drug therapy<br />
• Maternal substance abuse<br />
• Fetal Malformation<br />
• Diminished fetal activity<br />
• No prenatal care<br />
• Maternal age < 16 or > 35 years<br />
• Non-reassuring FHR patterns<br />
• Use of general anaesthesia<br />
• Uterine tetany<br />
• Narcotics to mum within 4 hours of<br />
delivery<br />
• Meconium-stained liquor<br />
• Prolapsed cord<br />
• Abruptio placentae<br />
• Placenta praevia<br />
While the Apgar score at birth may not be useful for decision-making at the<br />
beginning of resuscitation, it is helpful for assessing the infant’s condition and<br />
identifying the infant with a problem. Subsequent Apgar scores help in the<br />
assessment of the effectiveness of the resuscitative effort.