European Human Genetics Conference 2007 June 16 – 19, 2007 ...
European Human Genetics Conference 2007 June 16 – 19, 2007 ...
European Human Genetics Conference 2007 June 16 – 19, 2007 ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Cancer genetics<br />
low: 8% (8/98 samples). Loss of heterozygosity (LOH) study with the<br />
intragenic microsatellite marker D9S313 revealed LAMC3 locus deletions<br />
in 8/48 (17%) breast cancer samples. Methylation and LOH<br />
studies were also performed for bladder and clear cell renal cancers,<br />
demonstrating higher frequencies of LAMC3 molecular alterations.<br />
The study was supported in part by Applied Biosystems, USA.<br />
Molecular pathology of the LAMC3 gene in breast, renal and bladder cancers<br />
Total number of<br />
samples tested<br />
LOH<br />
Number (%)of<br />
hetero-zygotes<br />
Number (%) of<br />
samples with LOH<br />
Methylation Expression<br />
Breast cancer 58 48 (83%) 8 (17%) 8/98 (8%) 29/31 (94%)<br />
Clear cell renal<br />
cancer<br />
75 49 (65%) 10 (20%) 8/34 (24%) n/a<br />
Bladder cancer 77 45 (58%) 12 (27%) 13/45 (29%) n/a<br />
P0570. Angiotensin Converting Enzyme (ACE) Insertion/Deletion<br />
(I/D) Gene Polymorphisms in Leukemic Hematopoiesis<br />
I. Akalin 1 , E. Koca 2 , H. G. Karabulut 1 , D. Cetiner 2 , I. C. Haznedaroglu 2 , M.<br />
Hayran 3 , I. K. Onal 4 , O. I. Ozcebe 2 , A. Tukun 1 ;<br />
1 Ankara University Faculty of Medicine, Department of Medical <strong>Genetics</strong>,<br />
Ankara, Turkey, 2 Hacettepe University Medical School, Department of Internal<br />
Medicine, Hematology Division, Ankara, Turkey, 3 Hacettepe University Medical<br />
School, Department of Preventive Oncology, Ankara, Turkey, 4 Hacettepe University<br />
Medical School, Department of Internal Medicine, Ankara, Turkey.<br />
Renin angiotensin system (RAS) represents an autocrin/paracrin system<br />
affecting normal and neoplastic hematopoiesis. In this study, we<br />
investigated angiotensin converting enzyme (ACE) insertion/deletion<br />
(I/D) gene polymorphisms, which may affect the behavior of the local<br />
RAS in hematological neoplastic disorders.<br />
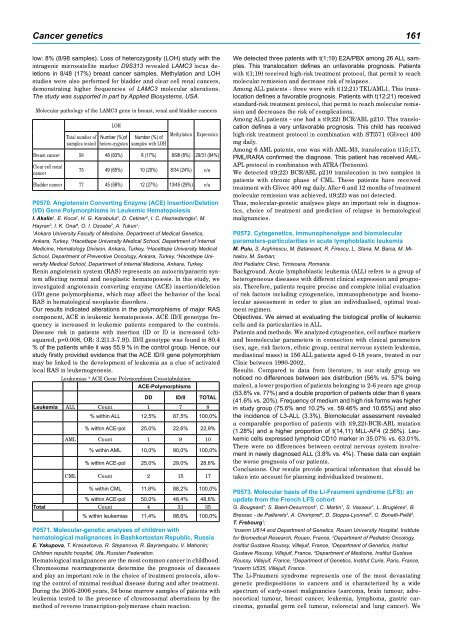
Our results indicated alterations in the polymorphisms of major RAS<br />
component, ACE in leukemic hematopoiesis. ACE ID/II genotype frequency<br />
is increased in leukemic patients compared to the controls.<br />
Disease risk in patients with insertion (ID or II) is increased (chisquared,<br />
p=0.008, OR: 3.2[1.3-7.9]). ID/II genotype was found in 80.4<br />
% of the patients while it was 55.9 % in the control group. Hence, our<br />
study firstly provided evidence that the ACE ID/II gene polymorphism<br />
may be linked to the development of leukemia as a clue of activated<br />
local RAS in leukemogenesis.<br />
Leukemias * ACE Gene Polymorphism Crosstabulation<br />
ACE-Polymorphisms<br />
DD ID/II TOTAL<br />
Leukemia ALL Count 1 7 8<br />
% within ALL 12,5% 87,5% 100,0%<br />
% within ACE-pol 25,0% 22,6% 22,9%<br />
AML Count 1 9 10<br />
% within AML 10,0% 90,0% 100,0%<br />
% within ACE-pol 25,0% 29,0% 28,6%<br />
CML Count 2 15 17<br />
% within CML 11,8% 88,2% 100,0%<br />
% within ACE-pol 50,0% 48,4% 48,6%<br />
Total Count 4 31 35<br />
% within leukemias 11,4% 88,6% 100,0%<br />
P0571. Molecular-genetic analyses of children with<br />
hematological malignances in Bashkortostan Republic, Russia<br />
E. Yakupova, T. Krasavtceva, R. Stepanova, R. Bayramgulov, V. Mahonin;<br />
Children republic hospital, Ufa, Russian Federation.<br />
Hematological malignances are the most common cancer in childhood.<br />
Chromosome rearrangements determine the prognosis of diseases<br />
and play an important role in the choice of treatment protocols, allowing<br />
the control of minimal residual disease during and after treatment.<br />
During the 2005-2006 years, 34 bone marrow samples of patients with<br />
leukemia tested to the presence of chromosomal aberrations by the<br />
method of reverse transcription-polymerase chain reaction.<br />
1 1<br />
We detected three patents with t(1;<strong>19</strong>) E2A/PBX among 26 ALL samples.<br />
This translocation defines an unfavorable prognosis. Patients<br />
with t(1;<strong>19</strong>) received high-risk treatment protocol, that permit to reach<br />
molecular remission and decrease risk of relapses.<br />
Among ALL patients - three were with t(12;21) TEL/AML1. This translocation<br />
defines a favorable prognosis. Patients with t(12;21) received<br />
standard-risk treatment protocol, that permit to reach molecular remission<br />
and decreases the risk of complications.<br />
Among ALL patients - one had a t(9;22) BCR/ABL p210. This translocation<br />
defines a very unfavorable prognosis. This child has received<br />
high-risk treatment protocol in combination with STI571 (Glivec) 400<br />
mg daily.<br />
Among 6 AML patents, one was with AML-M3, translocation t(15;17),<br />
PML/RARA confirmed the diagnose. This patient has received AML-<br />
APL protocol in combination with ATRA (Tretionin).<br />
We detected t(9;22) BCR/ABL p210 translocation in two samples in<br />
patients with chronic phase of CML. These patients have received<br />
treatment with Glivec 400 mg daily. After 6 and 12 months of treatment<br />
molecular remission was achieved, t(9;22) was not detected.<br />
Thus, molecular-genetic analyses plays an important role in diagnostics,<br />
choice of treatment and prediction of relapse in hematological<br />
malignancies.<br />
P0572. Cytogenetics, immunophenotype and biomolecular<br />
parameters-particularities in acute lymphoblastic leukemia<br />
M. Puiu, S. Arghirescu, M. Bataneant, R. Firescu, L. Stana, M. Baica, M. Mihailov,<br />
M. Serban;<br />
IIIrd Pediatric Clinic, Timisoara, Romania.<br />
Background. Acute lymphoblastic leukemia (ALL) refers to a group of<br />
heterogeneous diseases with different clinical expression and prognosis.<br />
Therefore, patients require precise and complete initial evaluation<br />
of risk factors including cytogenetics, immunophenotype and biomolecular<br />
assessment in order to plan an individualised, optimal treatment<br />
regimen.<br />
Objectives. We aimed at evaluating the biological profile of leukemic<br />
cells and its particularities in ALL.<br />
Patients and methods. We analyzed cytogenetics, cell surface markers<br />
and biomolecular parameters in connection with clinical parameters<br />
(sex, age, risk factors, ethnic group, central nervous system leukemia,<br />
mediastinal mass) in 156 ALL patients aged 0-18 years, treated in our<br />
Clinic between <strong>19</strong>90-2002.<br />
Results. Compared to data from literature, in our study group we<br />
noticed no differences between sex distribution (56% vs. 57% being<br />
males), a lower proportion of patients belonging to 2-6 years age group<br />
(53.8% vs. 77%) and a double proportion of patients older than 6 years<br />
(41.6% vs. 20%). Frequency of medium and high risk forms was higher<br />
in study group (75.6% and 10.2% vs. 59.46% and 10.65%) and also<br />
the incidence of L3-ALL (3.3%). Biomolecular assessment revealed<br />
a comparable proportion of patients with t(9,22)-BCR-ABL mutation<br />
(1.28%) and a higher proportion of t(14,11) MLL-AF4 (2.56%). Leukemic<br />
cells expressed lymphoid CD10 marker in 35.07% vs. 63.01%.<br />
There were no differences between central nervous system involvement<br />
in newly diagnosed ALL (3.8% vs. 4%). These data can explain<br />
the worse prognosis of our patients.<br />
Conclusions. Our results provide practical information that should be<br />
taken into account for planning individualized treatment.<br />
P0573. Molecular basis of the Li-Fraumeni syndrome (LFS): an<br />
update from the French LFS cohort<br />
G. Bougeard 1 , S. Baert-Desurmont 1 , C. Martin 1 , S. Vasseur 1 , L. Brugières 2 , B.<br />
Bressac - de Paillerets 3 , A. Chompret 4 , D. Stoppa-Lyonnet 5 , C. Bonaïti-Pellé 6 ,<br />
T. Frebourg 1 ;<br />
1 Inserm U614 and Department of <strong>Genetics</strong>, Rouen University Hospital, Institute<br />
for Biomedical Research, Rouen, France, 2 Department of Pediatric Oncology,<br />
Institut Gustave Roussy, Villejuif, France, 3 Department of <strong>Genetics</strong>, Institut<br />
Gustave Roussy, Villejuif, France, 4 Department of Medicine, Institut Gustave<br />
Roussy, Villejuif, France, 5 Department of <strong>Genetics</strong>, Institut Curie, Paris, France,<br />
6 Inserm U535, Villejuif, France.<br />
The Li-Fraumeni syndrome represents one of the most devastating<br />
genetic predispositions to cancers and is characterized by a wide<br />
spectrum of early-onset malignancies (sarcoma, brain tumour, adrenocortical<br />
tumour, breast cancer, leukemia, lymphoma, gastric carcinoma,<br />
gonadal germ cell tumour, colorectal and lung cancer). We