World Hospitals and Health Services - International Hospital ...
World Hospitals and Health Services - International Hospital ...
World Hospitals and Health Services - International Hospital ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
opinion matters 9/30/05 12:39 Page 47<br />
OPINION MATTERS<br />
improving overall health.<br />
Disease management components include:<br />
➜ Population identification processes;<br />
➜ Evidence-based practice guidelines;<br />
➜ Collaborative practice models to include physician <strong>and</strong><br />
support-service providers;<br />
➜ Patient self-management education (may include<br />
primary prevention, behavior modification programmes,<br />
<strong>and</strong> compliance/surveillance);<br />
➜ Process <strong>and</strong> outcomes measurement, evaluation, <strong>and</strong><br />
management;<br />
➜ Routine reporting/feedback loop (may include<br />
communication with patient, physician, health plan <strong>and</strong><br />
ancillary providers, <strong>and</strong> practice profiling).<br />
Full service disease management programmes must<br />
include all six components. Programmes consisting of fewer<br />
components are Disease Management Support <strong>Services</strong><br />
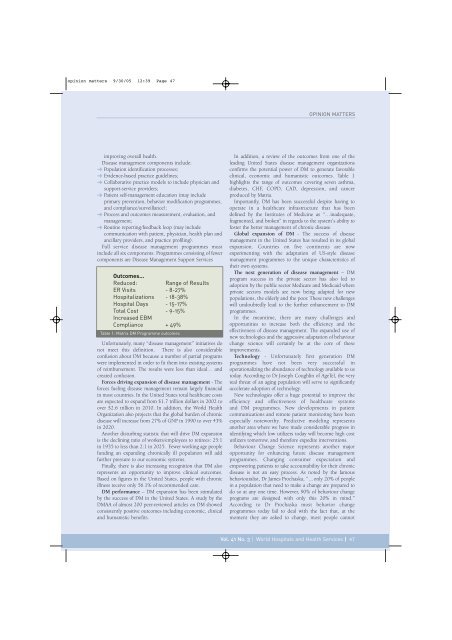
Outcomes…<br />
Reduced: Range of Results<br />
ER Visits - 8-27%<br />
<strong>Hospital</strong>izations - 18-38%<br />
<strong>Hospital</strong> Days - 15-17%<br />
Total Cost - 9-15%<br />
Increased EBM<br />
Compliance + 49%<br />
Table 1: Matria DM Programme outcomes<br />
Unfortunately, many “disease management” initiatives do<br />
not meet this definition. There is also considerable<br />
confusion about DM because a number of partial programs<br />
were implemented in order to fit them into existing systems<br />
of reimbursement. The results were less than ideal… <strong>and</strong><br />
created confusion.<br />
Forces driving expansion of disease management - The<br />
forces fueling disease management remain largely financial<br />
in most countries. In the United States total healthcare costs<br />
are expected to exp<strong>and</strong> from $1.7 trillion dollars in 2002 to<br />
over $2.6 trillion in 2010. In addition, the <strong>World</strong> <strong>Health</strong><br />
Organization also projects that the global burden of chronic<br />
disease will increase from 27% of GNP in 1990 to over 43%<br />
in 2020.<br />
Another disturbing statistic that will drive DM expansion<br />
is the declining ratio of workers/employees to retirees: 25:1<br />
in 1935 to less than 2:1 in 2025. Fewer working age people<br />
funding an exp<strong>and</strong>ing chronically ill population will add<br />
further pressure to our economic systems.<br />
Finally, there is also increasing recognition that DM also<br />
represents an opportunity to improve clinical outcomes.<br />
Based on figures in the United States, people with chronic<br />
illness receive only 56.1% of recommended care.<br />
DM performance – DM expansion has been stimulated<br />
by the success of DM in the United States. A study by the<br />
DMAA of almost 200 peer-reviewed articles on DM showed<br />
consistently positive outcomes including economic, clinical<br />
<strong>and</strong> humanistic benefits.<br />
In addition, a review of the outcomes from one of the<br />
leading United States disease management organizations<br />
confirms the potential power of DM to generate favorable<br />
clinical, economic <strong>and</strong> humanistic outcomes. Table 1<br />
highlights the range of outcomes covering seven asthma,<br />
diabetes, CHF, COPD, CAD, depression, <strong>and</strong> cancer<br />
produced by Matria.<br />
Importantly, DM has been successful despite having to<br />
operate in a healthcare infrastructure that has been<br />
defined by the Institutes of Medicine as “…inadequate,<br />
fragmented, <strong>and</strong> broken” in regards to the system’s ability to<br />
foster the better management of chronic disease.<br />
Global expansion of DM - The success of disease<br />
management in the United States has resulted in its global<br />
expansion. Countries on five continents are now<br />
experimenting with the adaptation of US-style disease<br />
management programmes to the unique characteristics of<br />
their own systems.<br />
The next generation of disease management – DM<br />
program success in the private sector has also led to<br />
adoption by the public sector Medicare <strong>and</strong> Medicaid where<br />
private sectors models are now being adapted for new<br />
populations, the elderly <strong>and</strong> the poor. These new challenges<br />
will undoubtedly lead to the further enhancement to DM<br />
programmes.<br />
In the meantime, there are many challenges <strong>and</strong><br />
opportunities to increase both the efficiency <strong>and</strong> the<br />
effectiveness of disease management. The exp<strong>and</strong>ed use of<br />
new technologies <strong>and</strong> the aggressive adaptation of behaviour<br />
change science will certainly be at the core of these<br />
improvements.<br />
Technology - Unfortunately first generation DM<br />
programmes have not been very successful in<br />
operationalizing the abundance of technology available to us<br />
today. According to Dr Joseph Coughlin of AgeTel, the very<br />
real threat of an aging population will serve to significantly<br />
accelerate adoption of technology.<br />
New technologies offer a huge potential to improve the<br />
efficiency <strong>and</strong> effectiveness of healthcare systems<br />
<strong>and</strong> DM programmes. New developments in patient<br />
communications <strong>and</strong> remote patient monitoring have been<br />
especially noteworthy. Predictive modeling represents<br />
another area where we have made considerable progress in<br />
identifying which low utilizers today will become high cost<br />
utilizers tomorrow, <strong>and</strong> therefore expedite interventions.<br />
Behaviour Change Science represents another major<br />
opportunity for enhancing future disease management<br />
programmes. Changing consumer expectation <strong>and</strong><br />
empowering patients to take accountability for their chronic<br />
disease is not an easy process. As noted by the famous<br />
behaviouralist, Dr James Prochaska, “…only 20% of people<br />
in a population that need to make a change are prepared to<br />
do so at any one time. However, 90% of behaviour change<br />
programs are designed with only this 20% in mind.”<br />
According to Dr Prochaska most behavior change<br />
programmes today fail to deal with the fact that, at the<br />
moment they are asked to change, most people cannot<br />
Vol. 41 No. 3 | <strong>World</strong> <strong><strong>Hospital</strong>s</strong> <strong>and</strong> <strong>Health</strong> <strong>Services</strong> | 47