Public Health Nursing Documentation Guidelines - Indian Health ...
Public Health Nursing Documentation Guidelines - Indian Health ...
Public Health Nursing Documentation Guidelines - Indian Health ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Documentation</strong> and Coding <strong>Guidelines</strong> for <strong>Public</strong> <strong>Health</strong> Nurses<br />
entry, or patient business office. The Centers for Disease Control and Prevention has<br />
an entire Web site dedicated to the International Classification of Diseases at<br />
http://www.cdc.gov/nchs/icd.htm.<br />
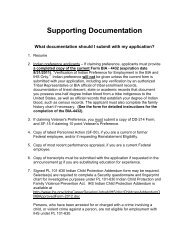
Nurses are sometimes reluctant to put a medical diagnosis on the PCC. However, if<br />
a medical diagnosis—for instance, diabetes—has already been made by a physician,<br />
then the nurse is not making his or her own diagnosis if he or she writes “diabetes<br />
foot care” or “diabetes—knowledge deficit related to insulin administration.” In addition,<br />
because the purpose of visit represents the highest level of knowledge, it is appropriate<br />
for the nurse to document his or her level of knowledge (e.g., “papular, diffuse,<br />
rash”) without having to make a diagnosis of specific cause.<br />
Although primary data entry and retrieval is based on medical diagnosis, nursing<br />
diagnosis is still very appropriate and is encouraged for use in the purpose of visit<br />
section. The nursing diagnosis must include the phrase “related to” followed by the<br />
medical diagnosis. If the diagnosis is not definitely established—tuberculosis suspect,<br />
unconfirmed pregnancy, or possible strep throat—then the nurse should document<br />
symptoms rather than a diagnosis. For example, if unsure of the diagnosis,<br />
write “sore throat” instead of “possible strep throat.” The rule is to document the<br />
highest level of knowledge. So, if the client has abdominal pain and the cause is unknown,<br />
then write “abdominal pain,” not “possible gallbladder disease” or “rule out<br />
appendicitis.” The terms “rule out,” “possible,” “probable,” etc., should not be used in<br />
the purpose of visit field.<br />
The diagnosis, assessments, and problems documented in this section are printed<br />
verbatim in the Outpatient and Field Encounters section of the patient’s <strong>Health</strong><br />
Summary.<br />
<strong>Indian</strong> <strong>Health</strong> Service Page 6-6