RPS Conference 2010, Abstracts 2010 - Royal Pharmaceutical Society
RPS Conference 2010, Abstracts 2010 - Royal Pharmaceutical Society
RPS Conference 2010, Abstracts 2010 - Royal Pharmaceutical Society
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
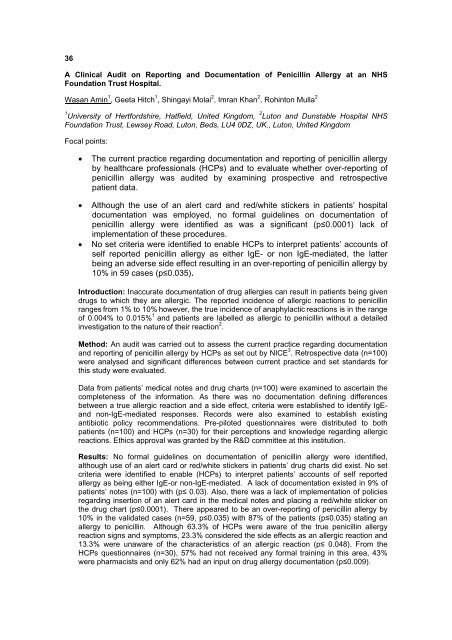
36<br />
A Clinical Audit on Reporting and Documentation of Penicillin Allergy at an NHS<br />
Foundation Trust Hospital.<br />
Wasan Amin 1 , Geeta Hitch 1 , Shingayi Molai 2 , Imran Khan 2 , Rohinton Mulla 2<br />
1 University of Hertfordshire, Hatfield, United Kingdom, 2 Luton and Dunstable Hospital NHS<br />
Foundation Trust, Lewsey Road, Luton, Beds, LU4 0DZ, UK., Luton, United Kingdom<br />
Focal points:<br />
• The current practice regarding documentation and reporting of penicillin allergy<br />
by healthcare professionals (HCPs) and to evaluate whether over-reporting of<br />
penicillin allergy was audited by examining prospective and retrospective<br />
patient data.<br />
• Although the use of an alert card and red/white stickers in patients’ hospital<br />
documentation was employed, no formal guidelines on documentation of<br />
penicillin allergy were identified as was a significant (p≤0.0001) lack of<br />
implementation of these procedures.<br />
• No set criteria were identified to enable HCPs to interpret patients’ accounts of<br />
self reported penicillin allergy as either IgE- or non IgE-mediated, the latter<br />
being an adverse side effect resulting in an over-reporting of penicillin allergy by<br />
10% in 59 cases (p≤0.035).<br />
Introduction: Inaccurate documentation of drug allergies can result in patients being given<br />
drugs to which they are allergic. The reported incidence of allergic reactions to penicillin<br />
ranges from 1% to 10% however, the true incidence of anaphylactic reactions is in the range<br />
of 0.004% to 0.015% 1 and patients are labelled as allergic to penicillin without a detailed<br />
investigation to the nature of their reaction 2 .<br />
Method: An audit was carried out to assess the current practice regarding documentation<br />
and reporting of penicillin allergy by HCPs as set out by NICE 3 . Retrospective data (n=100)<br />
were analysed and significant differences between current practice and set standards for<br />
this study were evaluated.<br />
Data from patients’ medical notes and drug charts (n=100) were examined to ascertain the<br />
completeness of the information. As there was no documentation defining differences<br />
between a true allergic reaction and a side effect, criteria were established to identify IgEand<br />
non-IgE-mediated responses. Records were also examined to establish existing<br />
antibiotic policy recommendations. Pre-piloted questionnaires were distributed to both<br />
patients (n=100) and HCPs (n=30) for their perceptions and knowledge regarding allergic<br />
reactions. Ethics approval was granted by the R&D committee at this institution.<br />
Results: No formal guidelines on documentation of penicillin allergy were identified,<br />
although use of an alert card or red/white stickers in patients’ drug charts did exist. No set<br />
criteria were identified to enable (HCPs) to interpret patients’ accounts of self reported<br />
allergy as being either IgE-or non-IgE-mediated. A lack of documentation existed in 9% of<br />
patients’ notes (n=100) with (p≤ 0.03). Also, there was a lack of implementation of policies<br />
regarding insertion of an alert card in the medical notes and placing a red/white sticker on<br />
the drug chart (p≤0.0001). There appeared to be an over-reporting of penicillin allergy by<br />
10% in the validated cases (n=59, p≤0.035) with 87% of the patients (p≤0.035) stating an<br />
allergy to penicillin. Although 63.3% of HCPs were aware of the true penicillin allergy<br />
reaction signs and symptoms, 23.3% considered the side effects as an allergic reaction and<br />
13.3% were unaware of the characteristics of an allergic reaction (p≤ 0.048). From the<br />
HCPs questionnaires (n=30), 57% had not received any formal training in this area, 43%<br />
were pharmacists and only 62% had an input on drug allergy documentation (p≤0.009).