Abstracts of the Academy of Dental Materials Annual ... - IsiRed
Abstracts of the Academy of Dental Materials Annual ... - IsiRed
Abstracts of the Academy of Dental Materials Annual ... - IsiRed
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
land); Thermafil: non-standardized 06-30 cones with plastic<br />
carrier heated in <strong>the</strong> Thermaprep Plus oven (Dentsply Maillefer,<br />
Baillagues, Switzerland). Following obturation, <strong>the</strong> two<br />
halves <strong>of</strong> each model were separated and photographed using<br />
a digital camera (Nikon ® D50 Macro lens with 105 mm f<br />
2.8). The gutta-percha filling ability was evaluated at 2, 4,<br />
6, and 8 mm from <strong>the</strong> established apex length by assigning<br />
<strong>the</strong> following scores: lateral grooves: 0 = absence <strong>of</strong> material,<br />
1 = presence <strong>of</strong> material; dentin depressions: 0 = absence <strong>of</strong><br />
material, 1 = partial filling, 2 = total filling. Scores at lateral<br />
grooves and dentin depressions were statistically compared<br />
among techniques at <strong>the</strong> same level and among levels within<br />
<strong>the</strong> same technique (Kruskal–Wallis ANOVA, Dunn’s Multiple<br />
Range test, p < 0.05).<br />
Results:<br />
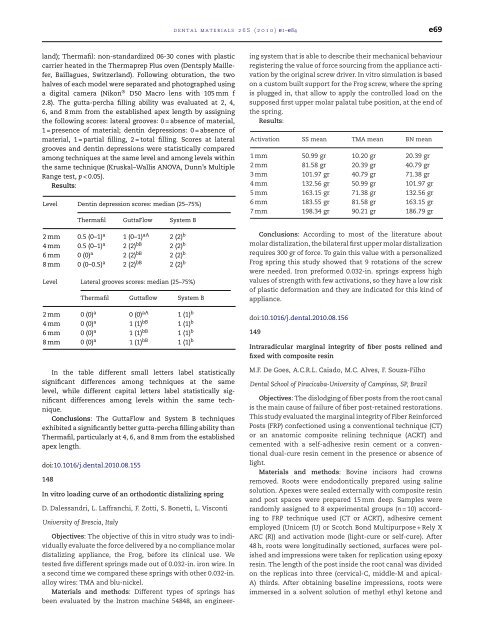
Level Dentin depression scores: median (25–75%)<br />
Thermafil GuttaFlow System B<br />
2 mm 0.5 (0–1) a 1 (0–1) aA 2 (2) b<br />
4 mm 0.5 (0–1) a 2 (2) bB 2 (2) b<br />
6 mm 0 (0) a 2 (2) bB 2 (2) b<br />
8 mm 0 (0–0.5) a 2 (2) bB 2 (2) b<br />
Level Lateral grooves scores: median (25–75%)<br />
Thermafil Guttaflow System B<br />
2 mm 0 (0) a 0 (0) aA 1 (1) b<br />
4 mm 0 (0) a 1 (1) bB 1 (1) b<br />
6 mm 0 (0) a 1 (1) bB 1 (1) b<br />
8 mm 0 (0) a 1 (1) bB 1 (1) b<br />
In <strong>the</strong> table different small letters label statistically<br />
significant differences among techniques at <strong>the</strong> same<br />
level, while different capital letters label statistically significant<br />
differences among levels within <strong>the</strong> same technique.<br />
Conclusions: The GuttaFlow and System B techniques<br />
exhibited a significantly better gutta-percha filling ability than<br />
Thermafil, particularly at 4, 6, and 8 mm from <strong>the</strong> established<br />
apex length.<br />
doi:10.1016/j.dental.2010.08.155<br />
148<br />
In vitro loading curve <strong>of</strong> an orthodontic distalizing spring<br />
D. Dalessandri, L. Laffranchi, F. Zotti, S. Bonetti, L. Visconti<br />
University <strong>of</strong> Brescia, Italy<br />
Objectives: The objective <strong>of</strong> this in vitro study was to individually<br />
evaluate <strong>the</strong> force delivered by a no compliance molar<br />
distalizing appliance, <strong>the</strong> Frog, before its clinical use. We<br />
tested five different springs made out <strong>of</strong> 0.032-in. iron wire. In<br />
a second time we compared <strong>the</strong>se springs with o<strong>the</strong>r 0.032-in.<br />
alloy wires: TMA and blu-nickel.<br />
<strong>Materials</strong> and methods: Different types <strong>of</strong> springs has<br />
been evaluated by <strong>the</strong> Instron machine 54848, an engineer-<br />
dental materials 26S (2010) e1–e84 e69<br />
ing system that is able to describe <strong>the</strong>ir mechanical behaviour<br />
registering <strong>the</strong> value <strong>of</strong> force sourcing from <strong>the</strong> appliance activation<br />
by <strong>the</strong> original screw driver. In vitro simulation is based<br />
on a custom built support for <strong>the</strong> Frog screw, where <strong>the</strong> spring<br />
is plugged in, that allow to apply <strong>the</strong> controlled load on <strong>the</strong><br />
supposed first upper molar palatal tube position, at <strong>the</strong> end <strong>of</strong><br />
<strong>the</strong> spring.<br />
Results:<br />
Activation SS mean TMA mean BN mean<br />
1 mm 50.99 gr 10.20 gr 20.39 gr<br />
2 mm 81.58 gr 20.39 gr 40.79 gr<br />
3 mm 101.97 gr 40.79 gr 71.38 gr<br />
4 mm 132.56 gr 50.99 gr 101.97 gr<br />
5 mm 163.15 gr 71.38 gr 132.56 gr<br />
6 mm 183.55 gr 81.58 gr 163.15 gr<br />
7 mm 198.34 gr 90.21 gr 186.79 gr<br />
Conclusions: According to most <strong>of</strong> <strong>the</strong> literature about<br />
molar distalization, <strong>the</strong> bilateral first upper molar distalization<br />
requires 300 gr <strong>of</strong> force. To gain this value with a personalized<br />
Frog spring this study showed that 9 rotations <strong>of</strong> <strong>the</strong> screw<br />
were needed. Iron preformed 0.032-in. springs express high<br />
values <strong>of</strong> strength with few activations, so <strong>the</strong>y have a low risk<br />
<strong>of</strong> plastic deformation and <strong>the</strong>y are indicated for this kind <strong>of</strong><br />
appliance.<br />
doi:10.1016/j.dental.2010.08.156<br />
149<br />
Intraradicular marginal integrity <strong>of</strong> fiber posts relined and<br />
fixed with composite resin<br />
M.F. De Goes, A.C.R.L. Caiado, M.C. Alves, F. Souza-Filho<br />
<strong>Dental</strong> School <strong>of</strong> Piracicaba-University <strong>of</strong> Campinas, SP, Brazil<br />
Objectives: The dislodging <strong>of</strong> fiber posts from <strong>the</strong> root canal<br />
is <strong>the</strong> main cause <strong>of</strong> failure <strong>of</strong> fiber post-retained restorations.<br />
This study evaluated <strong>the</strong> marginal integrity <strong>of</strong> Fiber Reinforced<br />
Posts (FRP) confectioned using a conventional technique (CT)<br />
or an anatomic composite relining technique (ACRT) and<br />
cemented with a self-adhesive resin cement or a conventional<br />
dual-cure resin cement in <strong>the</strong> presence or absence <strong>of</strong><br />
light.<br />
<strong>Materials</strong> and methods: Bovine incisors had crowns<br />
removed. Roots were endodontically prepared using saline<br />
solution. Apexes were sealed externally with composite resin<br />
and post spaces were prepared 15 mm deep. Samples were<br />
randomly assigned to 8 experimental groups (n = 10) according<br />
to FRP technique used (CT or ACRT), adhesive cement<br />
employed (Unicem (U) or Scotch Bond Multipurpose + Rely X<br />
ARC (R)) and activation mode (light-cure or self-cure). After<br />
48 h, roots were longitudinally sectioned, surfaces were polished<br />
and impressions were taken for replication using epoxy<br />
resin. The length <strong>of</strong> <strong>the</strong> post inside <strong>the</strong> root canal was divided<br />
on <strong>the</strong> replicas into three (cervical-C, middle-M and apical-<br />
A) thirds. After obtaining baseline impressions, roots were<br />
immersed in a solvent solution <strong>of</strong> methyl ethyl ketone and