Congenital malformations - Edocr
Congenital malformations - Edocr
Congenital malformations - Edocr
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
CHAPTER 37 OMPHALOCELE 243<br />
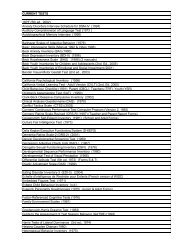
TABLE 37-1 Common <strong>Congenital</strong><br />
Malformations in Infants with Omphalocele<br />
and a Normal Karyotype<br />
Central nervous system<br />
• Spinal defects<br />
• Anencephaly<br />
• Craniosynostosis<br />
Cardiovascular system<br />
• Ventricular septal defect<br />
• Atrial septal defect<br />
• Tetralogy of Fallot<br />
• Coarctation of aorta<br />
• Persistent pulmonary hypertension of<br />
newborn<br />
Genitourinary system<br />
• Renal agenesis<br />
• Hypospadias<br />
Others<br />
• Skeletal dysplasia<br />
• Arthrogryposis<br />
• Diaphragmatic hernia<br />
• Cystic hygroma<br />
except those directly related to the defect such as<br />
malrotation of the gut, pulmonary hypoplasia. Associated<br />
chromosomal abnormalities are rare in<br />
infants with isolated omphalocele but nearly<br />
half of all omphalocele infants with other structural<br />
anomalies have an associated chromosomal<br />
abnormality. 5,6 The commonly associated<br />
structural anomalies in omphalocele infants with<br />
a normal karyotype are listed in Table 37-1. The<br />
likelihood of associated <strong>malformations</strong> is higher<br />
in infants with a larger omphalocele.<br />
According to the Online Mendelian Inheritance<br />
in Man (OMIM) database, >50 syndromes<br />
have been described in association with omphalocele.<br />
Chromosomal abnormalities have been<br />
reported in 20–60% of all liveborn infants with<br />
omphalocele. The most frequently associated syndromes<br />
are Beckwith-Wiedemann syndrome and<br />
trisomy 13 and 18. The other commonly associated<br />
syndromes are listed in Table 37-2. Associated<br />
chromosomal abnormalities are more likely<br />
in infants with small omphalocele with intracorporeal<br />
liver. 1<br />
EVALUATION<br />
Prenatal diagnosis of omphalocele is easy and<br />
fairly common. Maternal serum alpha-fetoprotein<br />
(MSAFP) level is elevated in majority of fetuses<br />
with omphalocele and nearly all infants can be diagnosed<br />
on prenatal ultrasound. However, it is<br />
important to remember that the late first trimester<br />
ultrasound can result in an erroneous diagnosis of<br />
abdominal wall defects because of normal physiologic<br />
herniation of bowel into the base of the<br />
umbilical cord. Amniocentesis for karyotype, prenatal<br />
echocardiography, and detailed ultrasonography<br />
evaluation for associated <strong>malformations</strong><br />
should be offered as soon as possible after a prenatal<br />
diagnosis of omphalocele is made. All infants<br />
should undergo echocardiography after birth<br />
to exclude any congenital cardiac abnormalities<br />
and karyotype should be obtained if not done<br />
prenatally. The need for a cranial or a renal ultrasound<br />
is less clear in the absence of any associated<br />
<strong>malformations</strong> on clinical exam and cardiac<br />
echo. Infants with Beckwith-Wiedemann syndrome<br />
should be monitored for ongoing episodes<br />
of hypoglycemia and should have kayotype and<br />
methylation testing of chromosome 11p15.<br />
MANAGEMENT AND PROGNOSIS<br />
In several studies and meta-analyses, the mode of<br />
delivery has not been shown to affect either survival<br />
or morbidity in these infants. 7 All infants with<br />
omphalocele should be carefully examined after<br />
birth for the presence of associated anomalies and<br />
clues to associated syndromes such as Beckwith-<br />
Wiedemann syndrome. Serum blood sugar should<br />
be monitored closely to exclude hypoglycemia<br />
which is commonly seen in infants with Beckwith-<br />
Wiedemann syndrome. These infants should also<br />
be monitored closely after birth for signs of pulmonary<br />
insufficiency and persistent pulmonary<br />
hypertension of newborn. Primary repair and closure<br />
of abdominal wall defect is the procedure of<br />
choice but placement of silo and sequential reductions<br />
are offered to infants with larger defects in<br />
whom primary repair can compromise pulmonary