Congenital malformations - Edocr
Congenital malformations - Edocr
Congenital malformations - Edocr
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
72 PART II CENTRAL NERVOUS SYSTEM MALFORMATIONS<br />
CLINICAL PRESENTATION<br />
The Chiari I malformation is rarely diagnosed in<br />
the neonatal period unless it is associated with a<br />
broader malformation syndrome that leads to<br />
neuroimaging. Patients with an isolated Chiari I<br />
typically appear normal in early infancy and the<br />
diagnosis is not established until early adult life. At<br />
the time of diagnosis, it is sometimes recognized,<br />
however, that patients have had lifelong symptoms<br />
including headache and clumsiness. When<br />
the diagnosis is established, the most common<br />
presenting symptoms are headache and neck pain,<br />
although a wide variety of signs and symptoms<br />
can be observed. 5 Symptoms in Chiari I are generally<br />
felt to be the result of direct cerebellar<br />
compromise, compression of the brain stem and<br />
cranial nerves, and syrinx-associated central cord<br />
syndrome. In addition to head and neck pain,<br />
other symptoms that can be observed include<br />
blurred vision or photophobia, dizziness, tinnitus,<br />
decreased hearing, dysphagia, numbness, and<br />
weakness. Some patients present with apnea, possibly<br />
related to respiratory center dysfunction, or<br />
to vocal cord paralysis, and these patients may be<br />
at increased risk for postoperative complications.<br />
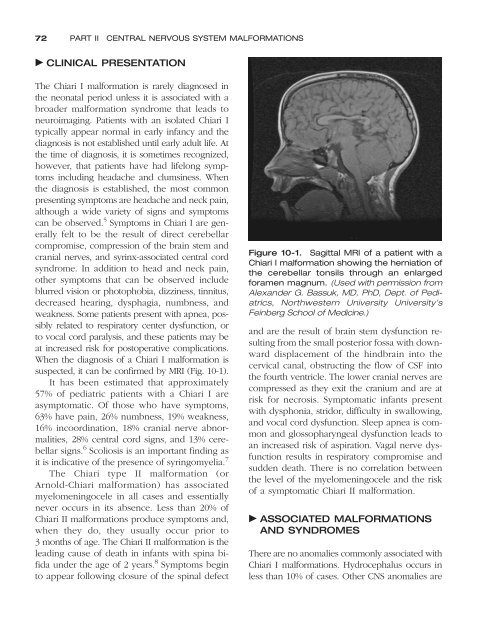
When the diagnosis of a Chiari I malformation is<br />
suspected, it can be confirmed by MRI (Fig. 10-1).<br />
It has been estimated that approximately<br />
57% of pediatric patients with a Chiari I are<br />
asymptomatic. Of those who have symptoms,<br />
63% have pain, 26% numbness, 19% weakness,<br />
16% incoordination, 18% cranial nerve abnormalities,<br />
28% central cord signs, and 13% cerebellar<br />
signs. 6 Scoliosis is an important finding as<br />
it is indicative of the presence of syringomyelia. 7<br />
The Chiari type II malformation (or<br />
Arnold-Chiari malformation) has associated<br />
myelomeningocele in all cases and essentially<br />
never occurs in its absence. Less than 20% of<br />
Chiari II <strong>malformations</strong> produce symptoms and,<br />
when they do, they usually occur prior to<br />
3 months of age. The Chiari II malformation is the<br />
leading cause of death in infants with spina bifida<br />
under the age of 2 years. 8 Symptoms begin<br />
to appear following closure of the spinal defect<br />
Figure 10-1. Sagittal MRI of a patient with a<br />
Chiari I malformation showing the herniation of<br />
the cerebellar tonsils through an enlarged<br />
foramen magnum. (Used with permission from<br />
Alexander G. Bassuk, MD, PhD, Dept. of Pediatrics,<br />
Northwestern University University’s<br />
Feinberg School of Medicine.)<br />
and are the result of brain stem dysfunction resulting<br />
from the small posterior fossa with downward<br />
displacement of the hindbrain into the<br />
cervical canal, obstructing the flow of CSF into<br />
the fourth ventricle. The lower cranial nerves are<br />
compressed as they exit the cranium and are at<br />
risk for necrosis. Symptomatic infants present<br />
with dysphonia, stridor, difficulty in swallowing,<br />
and vocal cord dysfunction. Sleep apnea is common<br />
and glossopharyngeal dysfunction leads to<br />
an increased risk of aspiration. Vagal nerve dysfunction<br />
results in respiratory compromise and<br />
sudden death. There is no correlation between<br />
the level of the myelomeningocele and the risk<br />
of a symptomatic Chiari II malformation.<br />
ASSOCIATED MALFORMATIONS<br />
AND SYNDROMES<br />
There are no anomalies commonly associated with<br />
Chiari I <strong>malformations</strong>. Hydrocephalus occurs in<br />
less than 10% of cases. Other CNS anomalies are