Immunotherapy Safety for the Primary Care ... - U.S. Coast Guard
Immunotherapy Safety for the Primary Care ... - U.S. Coast Guard
Immunotherapy Safety for the Primary Care ... - U.S. Coast Guard
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
S46 Cox et al<br />
J ALLERGY CLIN IMMUNOL<br />
SEPTEMBER 2007<br />
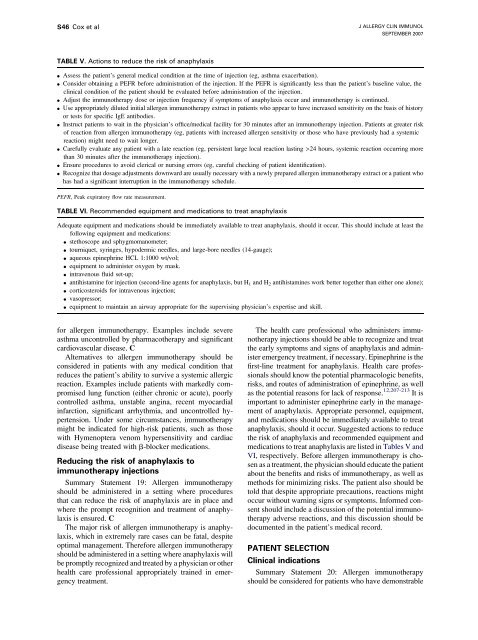
TABLE V. Actions to reduce <strong>the</strong> risk of anaphylaxis<br />
d<br />
d<br />
d<br />
d<br />
d<br />
d<br />
d<br />
d<br />
Assess <strong>the</strong> patient’s general medical condition at <strong>the</strong> time of injection (eg, asthma exacerbation).<br />
Consider obtaining a PEFR be<strong>for</strong>e administration of <strong>the</strong> injection. If <strong>the</strong> PEFR is significantly less than <strong>the</strong> patient’s baseline value, <strong>the</strong><br />
clinical condition of <strong>the</strong> patient should be evaluated be<strong>for</strong>e administration of <strong>the</strong> injection.<br />
Adjust <strong>the</strong> immuno<strong>the</strong>rapy dose or injection frequency if symptoms of anaphylaxis occur and immuno<strong>the</strong>rapy is continued.<br />
Use appropriately diluted initial allergen immuno<strong>the</strong>rapy extract in patients who appear to have increased sensitivity on <strong>the</strong> basis of history<br />
or tests <strong>for</strong> specific IgE antibodies.<br />
Instruct patients to wait in <strong>the</strong> physician’s office/medical facility <strong>for</strong> 30 minutes after an immuno<strong>the</strong>rapy injection. Patients at greater risk<br />
of reaction from allergen immuno<strong>the</strong>rapy (eg, patients with increased allergen sensitivity or those who have previously had a systemic<br />
reaction) might need to wait longer.<br />
<strong>Care</strong>fully evaluate any patient with a late reaction (eg, persistent large local reaction lasting >24 hours, systemic reaction occurring more<br />
than 30 minutes after <strong>the</strong> immuno<strong>the</strong>rapy injection).<br />
Ensure procedures to avoid clerical or nursing errors (eg, careful checking of patient identification).<br />
Recognize that dosage adjustments downward are usually necessary with a newly prepared allergen immuno<strong>the</strong>rapy extract or a patient who<br />
has had a significant interruption in <strong>the</strong> immuno<strong>the</strong>rapy schedule.<br />
PEFR, Peak expiratory flow rate measurement.<br />
TABLE VI. Recommended equipment and medications to treat anaphylaxis<br />
Adequate equipment and medications should be immediately available to treat anaphylaxis, should it occur. This should include at least <strong>the</strong><br />
following equipment and medications:<br />
d stethoscope and sphygmomanometer;<br />
d tourniquet, syringes, hypodermic needles, and large-bore needles (14-gauge);<br />
d aqueous epinephrine HCL 1:1000 wt/vol;<br />
d equipment to administer oxygen by mask.<br />
d intravenous fluid set-up;<br />
d antihistamine <strong>for</strong> injection (second-line agents <strong>for</strong> anaphylaxis, but H 1 and H 2 antihistamines work better toge<strong>the</strong>r than ei<strong>the</strong>r one alone);<br />
d corticosteroids <strong>for</strong> intravenous injection;<br />
d vasopressor;<br />
d equipment to maintain an airway appropriate <strong>for</strong> <strong>the</strong> supervising physician’s expertise and skill.<br />
<strong>for</strong> allergen immuno<strong>the</strong>rapy. Examples include severe<br />
asthma uncontrolled by pharmaco<strong>the</strong>rapy and significant<br />
cardiovascular disease. C<br />
Alternatives to allergen immuno<strong>the</strong>rapy should be<br />
considered in patients with any medical condition that<br />
reduces <strong>the</strong> patient’s ability to survive a systemic allergic<br />
reaction. Examples include patients with markedly compromised<br />
lung function (ei<strong>the</strong>r chronic or acute), poorly<br />
controlled asthma, unstable angina, recent myocardial<br />
infarction, significant arrhythmia, and uncontrolled hypertension.<br />
Under some circumstances, immuno<strong>the</strong>rapy<br />
might be indicated <strong>for</strong> high-risk patients, such as those<br />
with Hymenoptera venom hypersensitivity and cardiac<br />
disease being treated with b-blocker medications.<br />
Reducing <strong>the</strong> risk of anaphylaxis to<br />
immuno<strong>the</strong>rapy injections<br />
Summary Statement 19: Allergen immuno<strong>the</strong>rapy<br />
should be administered in a setting where procedures<br />
that can reduce <strong>the</strong> risk of anaphylaxis are in place and<br />
where <strong>the</strong> prompt recognition and treatment of anaphylaxis<br />
is ensured. C<br />
The major risk of allergen immuno<strong>the</strong>rapy is anaphylaxis,<br />
which in extremely rare cases can be fatal, despite<br />
optimal management. There<strong>for</strong>e allergen immuno<strong>the</strong>rapy<br />
should be administered in a setting where anaphylaxis will<br />
be promptly recognized and treated by a physician or o<strong>the</strong>r<br />
health care professional appropriately trained in emergency<br />
treatment.<br />
The health care professional who administers immuno<strong>the</strong>rapy<br />
injections should be able to recognize and treat<br />
<strong>the</strong> early symptoms and signs of anaphylaxis and administer<br />
emergency treatment, if necessary. Epinephrine is <strong>the</strong><br />
first-line treatment <strong>for</strong> anaphylaxis. Health care professionals<br />
should know <strong>the</strong> potential pharmacologic benefits,<br />
risks, and routes of administration of epinephrine, as well<br />
as <strong>the</strong> potential reasons <strong>for</strong> lack of response. 12,207-213 It is<br />
important to administer epinephrine early in <strong>the</strong> management<br />
of anaphylaxis. Appropriate personnel, equipment,<br />
and medications should be immediately available to treat<br />
anaphylaxis, should it occur. Suggested actions to reduce<br />
<strong>the</strong> risk of anaphylaxis and recommended equipment and<br />
medications to treat anaphylaxis are listed in Tables V and<br />
VI, respectively. Be<strong>for</strong>e allergen immuno<strong>the</strong>rapy is chosen<br />
as a treatment, <strong>the</strong> physician should educate <strong>the</strong> patient<br />
about <strong>the</strong> benefits and risks of immuno<strong>the</strong>rapy, as well as<br />
methods <strong>for</strong> minimizing risks. The patient also should be<br />
told that despite appropriate precautions, reactions might<br />
occur without warning signs or symptoms. In<strong>for</strong>med consent<br />
should include a discussion of <strong>the</strong> potential immuno<strong>the</strong>rapy<br />
adverse reactions, and this discussion should be<br />
documented in <strong>the</strong> patient’s medical record.<br />
PATIENT SELECTION<br />
Clinical indications<br />
Summary Statement 20: Allergen immuno<strong>the</strong>rapy<br />
should be considered <strong>for</strong> patients who have demonstrable