Immunotherapy Safety for the Primary Care ... - U.S. Coast Guard
Immunotherapy Safety for the Primary Care ... - U.S. Coast Guard
Immunotherapy Safety for the Primary Care ... - U.S. Coast Guard
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
J ALLERGY CLIN IMMUNOL<br />
VOLUME 115, NUMBER 3<br />
Lieberman et al S491<br />
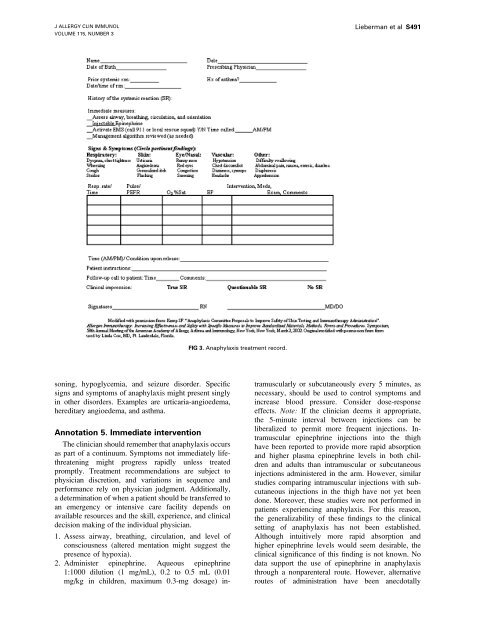
FIG 3. Anaphylaxis treatment record.<br />
soning, hypoglycemia, and seizure disorder. Specific<br />
signs and symptoms of anaphylaxis might present singly<br />
in o<strong>the</strong>r disorders. Examples are urticaria-angioedema,<br />
hereditary angioedema, and asthma.<br />
Annotation 5. Immediate intervention<br />
The clinician should remember that anaphylaxis occurs<br />
as part of a continuum. Symptoms not immediately lifethreatening<br />
might progress rapidly unless treated<br />
promptly. Treatment recommendations are subject to<br />
physician discretion, and variations in sequence and<br />
per<strong>for</strong>mance rely on physician judgment. Additionally,<br />
a determination of when a patient should be transferred to<br />
an emergency or intensive care facility depends on<br />
available resources and <strong>the</strong> skill, experience, and clinical<br />
decision making of <strong>the</strong> individual physician.<br />
1. Assess airway, breathing, circulation, and level of<br />
consciousness (altered mentation might suggest <strong>the</strong><br />
presence of hypoxia).<br />
2. Administer epinephrine. Aqueous epinephrine<br />
1:1000 dilution (1 mg/mL), 0.2 to 0.5 mL (0.01<br />
mg/kg in children, maximum 0.3-mg dosage) intramuscularly<br />
or subcutaneously every 5 minutes, as<br />
necessary, should be used to control symptoms and<br />
increase blood pressure. Consider dose-response<br />
effects. Note: If <strong>the</strong> clinician deems it appropriate,<br />
<strong>the</strong> 5-minute interval between injections can be<br />
liberalized to permit more frequent injections. Intramuscular<br />
epinephrine injections into <strong>the</strong> thigh<br />
have been reported to provide more rapid absorption<br />
and higher plasma epinephrine levels in both children<br />
and adults than intramuscular or subcutaneous<br />
injections administered in <strong>the</strong> arm. However, similar<br />
studies comparing intramuscular injections with subcutaneous<br />
injections in <strong>the</strong> thigh have not yet been<br />
done. Moreover, <strong>the</strong>se studies were not per<strong>for</strong>med in<br />
patients experiencing anaphylaxis. For this reason,<br />
<strong>the</strong> generalizability of <strong>the</strong>se findings to <strong>the</strong> clinical<br />
setting of anaphylaxis has not been established.<br />
Although intuitively more rapid absorption and<br />
higher epinephrine levels would seem desirable, <strong>the</strong><br />
clinical significance of this finding is not known. No<br />
data support <strong>the</strong> use of epinephrine in anaphylaxis<br />
through a nonparenteral route. However, alternative<br />
routes of administration have been anecdotally