Acupuncture and dry-needling for low back pain (Review)
Acupuncture and dry-needling for low back pain (Review)
Acupuncture and dry-needling for low back pain (Review)
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
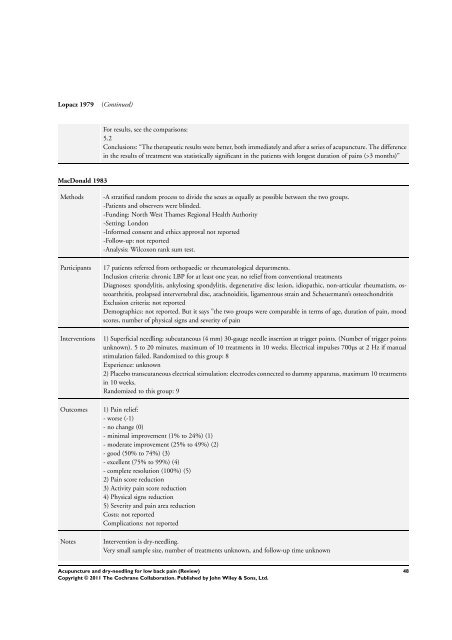
Lopacz 1979<br />
(Continued)<br />
For results, see the comparisons:<br />
5.2<br />
Conclusions: “The therapeutic results were better, both immediately <strong>and</strong> after a series of acupuncture. The difference<br />
in the results of treatment was statistically significant in the patients with longest duration of <strong>pain</strong>s (>3 months)”<br />
MacDonald 1983<br />
Methods<br />
Participants<br />
Interventions<br />
Outcomes<br />
Notes<br />
-A stratified r<strong>and</strong>om process to divide the sexes as equally as possible between the two groups.<br />
-Patients <strong>and</strong> observers were blinded.<br />
-Funding: North West Thames Regional Health Authority<br />
-Setting: London<br />
-In<strong>for</strong>med consent <strong>and</strong> ethics approval not reported<br />
-Fol<strong>low</strong>-up: not reported<br />
-Analysis: Wilcoxon rank sum test.<br />
17 patients referred from orthopaedic or rheumatological departments.<br />
Inclusion criteria: chronic LBP <strong>for</strong> at least one year, no relief from conventional treatments<br />
Diagnoses: spondylitis, ankylosing spondylitis, degenerative disc lesion, idiopathic, non-articular rheumatism, osteoarthritis,<br />
prolapsed intervertebral disc, arachnoiditis, ligamentous strain <strong>and</strong> Scheuermann’s osteochondritis<br />
Exclusion criteria: not reported<br />
Demographics: not reported. But it says ”the two groups were comparable in terms of age, duration of <strong>pain</strong>, mood<br />
scores, number of physical signs <strong>and</strong> severity of <strong>pain</strong><br />
1) Superficial <strong>needling</strong>: subcutaneous (4 mm) 30-gauge needle insertion at trigger points. (Number of trigger points<br />
unknown). 5 to 20 minutes, maximum of 10 treatments in 10 weeks. Electrical impulses 700µs at 2 Hz if manual<br />
stimulation failed. R<strong>and</strong>omized to this group: 8<br />
Experience: unknown<br />
2) Placebo transcutaneous electrical stimulation: electrodes connected to dummy apparatus, maximum 10 treatments<br />
in 10 weeks.<br />
R<strong>and</strong>omized to this group: 9<br />
1) Pain relief:<br />
- worse (-1)<br />
- no change (0)<br />
- minimal improvement (1% to 24%) (1)<br />
- moderate improvement (25% to 49%) (2)<br />
- good (50% to 74%) (3)<br />
- excellent (75% to 99%) (4)<br />
- complete resolution (100%) (5)<br />
2) Pain score reduction<br />
3) Activity <strong>pain</strong> score reduction<br />
4) Physical signs reduction<br />
5) Severity <strong>and</strong> <strong>pain</strong> area reduction<br />
Costs: not reported<br />
Complications: not reported<br />
Intervention is <strong>dry</strong>-<strong>needling</strong>.<br />
Very small sample size, number of treatments unknown, <strong>and</strong> fol<strong>low</strong>-up time unknown<br />
<strong>Acupuncture</strong> <strong>and</strong> <strong>dry</strong>-<strong>needling</strong> <strong>for</strong> <strong>low</strong> <strong>back</strong> <strong>pain</strong> (<strong>Review</strong>)<br />
Copyright © 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.<br />
48