Guidelines for a Palliative Approach in Residential Aged Care
Guidelines for a Palliative Approach in Residential Aged Care
Guidelines for a Palliative Approach in Residential Aged Care
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
therapy, blood glucose monitor<strong>in</strong>g, PEG/nasogastric feed<strong>in</strong>g, and unnecessary medications.<br />
There is no s<strong>in</strong>gle description of an <strong>in</strong>dividual’s last hours of life, and the aged care team needs<br />
to be alert to <strong>in</strong>dividual differences and the resident’s reactions to their impend<strong>in</strong>g death. The<br />
family may also require more support at this time and the aged care team needs to be able to<br />
provide this. The aged care team is <strong>in</strong> a unique position to assist families <strong>in</strong> cop<strong>in</strong>g with the loss<br />
of a relative dur<strong>in</strong>g the dy<strong>in</strong>g process and after death has occurred [373] (Level QE). This support<br />
may need to be practical as well as emotional [399] (Level QE). (See Chapters 8 ‘Family support’,<br />
and 15, ‘Bereavement support’, <strong>for</strong> further <strong>in</strong><strong>for</strong>mation).<br />
The follow<strong>in</strong>g story highlights some of the responses residents and their families may have when<br />
fac<strong>in</strong>g imm<strong>in</strong>ent death.<br />
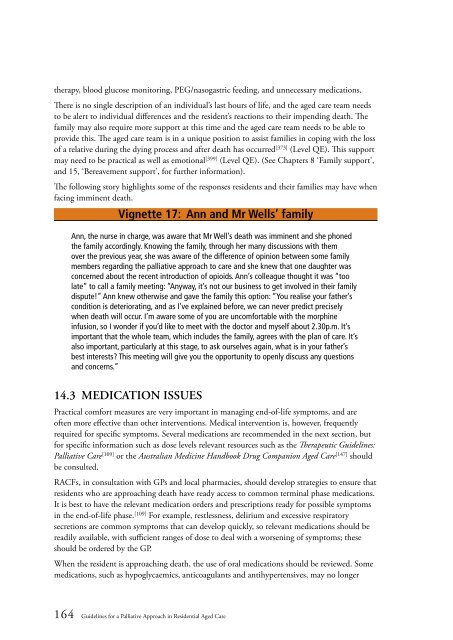
Vignette 17: Ann and Mr Wells’ family<br />
Ann, the nurse <strong>in</strong> charge, was aware that Mr Well’s death was imm<strong>in</strong>ent and she phoned<br />
the family accord<strong>in</strong>gly. Know<strong>in</strong>g the family, through her many discussions with them<br />
over the previous year, she was aware of the difference of op<strong>in</strong>ion between some family<br />
members regard<strong>in</strong>g the palliative approach to care and she knew that one daughter was<br />
concerned about the recent <strong>in</strong>troduction of opioids. Ann’s colleague thought it was “too<br />
late” to call a family meet<strong>in</strong>g: “Anyway, it’s not our bus<strong>in</strong>ess to get <strong>in</strong>volved <strong>in</strong> their family<br />
dispute!” Ann knew otherwise and gave the family this option: “You realise your father’s<br />
condition is deteriorat<strong>in</strong>g, and as I’ve expla<strong>in</strong>ed be<strong>for</strong>e, we can never predict precisely<br />
when death will occur. I’m aware some of you are uncom<strong>for</strong>table with the morph<strong>in</strong>e<br />
<strong>in</strong>fusion, so I wonder if you’d like to meet with the doctor and myself about 2.30p.m. It’s<br />
important that the whole team, which <strong>in</strong>cludes the family, agrees with the plan of care. It’s<br />
also important, particularly at this stage, to ask ourselves aga<strong>in</strong>, what is <strong>in</strong> your father’s<br />
best <strong>in</strong>terests? This meet<strong>in</strong>g will give you the opportunity to openly discuss any questions<br />
and concerns.”<br />
14.3 MEDICATION ISSUES<br />
Practical com<strong>for</strong>t measures are very important <strong>in</strong> manag<strong>in</strong>g end-of-life symptoms, and are<br />
often more effective than other <strong>in</strong>terventions. Medical <strong>in</strong>tervention is, however, frequently<br />
required <strong>for</strong> specific symptoms. Several medications are recommended <strong>in</strong> the next section, but<br />
<strong>for</strong> specific <strong>in</strong><strong>for</strong>mation such as dose levels relevant resources such as the Therapeutic <strong>Guidel<strong>in</strong>es</strong>:<br />
<strong>Palliative</strong> <strong>Care</strong> [109] or the Australian Medic<strong>in</strong>e Handbook Drug Companion <strong>Aged</strong> <strong>Care</strong> [147] should<br />
be consulted.<br />
RACFs, <strong>in</strong> consultation with GPs and local pharmacies, should develop strategies to ensure that<br />
residents who are approach<strong>in</strong>g death have ready access to common term<strong>in</strong>al phase medications.<br />
It is best to have the relevant medication orders and prescriptions ready <strong>for</strong> possible symptoms<br />
<strong>in</strong> the end-of-life phase. [109] For example, restlessness, delirium and excessive respiratory<br />
secretions are common symptoms that can develop quickly, so relevant medications should be<br />
readily available, with sufficient ranges of dose to deal with a worsen<strong>in</strong>g of symptoms; these<br />
should be ordered by the GP.<br />
When the resident is approach<strong>in</strong>g death, the use of oral medications should be reviewed. Some<br />
medications, such as hypoglycaemics, anticoagulants and antihypertensives, may no longer<br />
164 <strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> a <strong>Palliative</strong> <strong>Approach</strong> <strong>in</strong> <strong>Residential</strong> <strong>Aged</strong> <strong>Care</strong>