Guidelines for a Palliative Approach in Residential Aged Care
Guidelines for a Palliative Approach in Residential Aged Care
Guidelines for a Palliative Approach in Residential Aged Care
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
6.2.2 Barriers to effective pa<strong>in</strong> management<br />
The evidence suggests that lack of knowledge of pa<strong>in</strong> assessment among some nurses [127] (Level<br />
QE) and doctors [128] (Level EO) is contribut<strong>in</strong>g to poor pa<strong>in</strong> management of residents. An<br />
additional concern is the low level of knowledge of pa<strong>in</strong> management of some doctors, as they<br />
have had little <strong>for</strong>mal education <strong>in</strong> this area. [129–131] The literature cit<strong>in</strong>g these deficiencies calls<br />
<strong>for</strong> a collaborative approach between doctors and nurses to manage pa<strong>in</strong> consistently and well<br />
<strong>in</strong> the aged care sett<strong>in</strong>g [131] (Level QE). It also cites the need <strong>for</strong> educational programs that give<br />
def<strong>in</strong>itive and objective <strong>in</strong><strong>for</strong>mation on drugs [128,129] (Level EO; Level EO). Some practices have<br />
begun to change. These changes have <strong>in</strong>cluded improved education of doctors and nurses about<br />
pa<strong>in</strong> assessment and prescrib<strong>in</strong>g, development of more responsive assessment tools, improved<br />
treatment strategies, and better practices <strong>for</strong> monitor<strong>in</strong>g of residents’ pa<strong>in</strong> levels. [130] However,<br />
other barriers to effective pa<strong>in</strong> management still need to be addressed.<br />
There is some evidence that difficulties may be encountered when members of the aged care<br />
team lack the necessary skills <strong>for</strong> adequate report<strong>in</strong>g and also lack observation skills [90] (Level<br />
QE). Accurate report<strong>in</strong>g based on good observation skills is particularly important <strong>for</strong> those<br />
residents who do not articulate their pa<strong>in</strong> symptoms verbally and rely on a skilled person to<br />
assess their level of pa<strong>in</strong> based upon behavioural cues [132] (Level III-3).<br />
Effective pa<strong>in</strong> management may also be difficult <strong>for</strong> some residents due to their cultural beliefs.<br />
For example, a recent study found that <strong>in</strong> some Indigenous Australian communities there was<br />
considerable fear regard<strong>in</strong>g morph<strong>in</strong>e be<strong>in</strong>g given at the end of life [133] (Level QE). The common<br />
belief was that morph<strong>in</strong>e was the drug that was given to “get rid of me [them]”. [133, p. 146] This<br />
study also noted that many Indigenous Australians had a fear of needles and did not understand<br />
about drugs and palliative care. This study highlights the need to identify cultural issues <strong>for</strong> each<br />
resident <strong>in</strong> all aspects of care delivery. (See also Chapters 10, ‘Aborig<strong>in</strong>al and Torres Strait Islander<br />
Issues’ and 11, ‘Cultural issues’.)<br />
There is a large body of research demonstrat<strong>in</strong>g that some aged care team members may have<br />
misconceptions or myths about pa<strong>in</strong> management [128] (Level EO). These misconceptions can<br />
present major barriers to effective pa<strong>in</strong> management. The follow<strong>in</strong>g table provides an overview<br />
of some of these myths, and the facts <strong>in</strong> each case.<br />
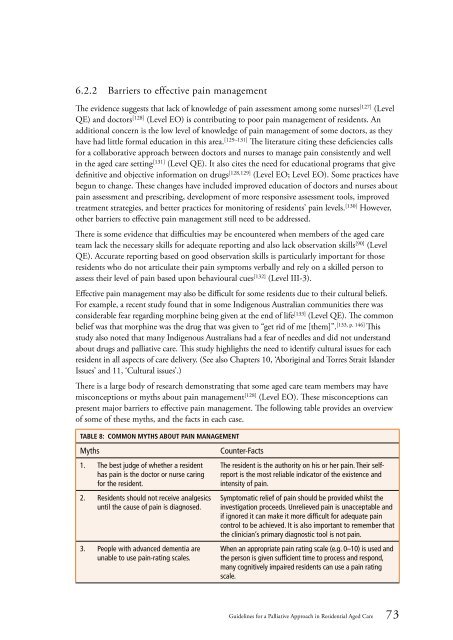
Table 8: Common myths about pa<strong>in</strong> management<br />
Myths<br />
1. The best judge of whether a resident<br />
has pa<strong>in</strong> is the doctor or nurse car<strong>in</strong>g<br />
<strong>for</strong> the resident.<br />
2. Residents should not receive analgesics<br />
until the cause of pa<strong>in</strong> is diagnosed.<br />
3. People with advanced dementia are<br />
unable to use pa<strong>in</strong>-rat<strong>in</strong>g scales.<br />
Counter-Facts<br />
The resident is the authority on his or her pa<strong>in</strong>. Their selfreport<br />
is the most reliable <strong>in</strong>dicator of the existence and<br />
<strong>in</strong>tensity of pa<strong>in</strong>.<br />
Symptomatic relief of pa<strong>in</strong> should be provided whilst the<br />
<strong>in</strong>vestigation proceeds. Unrelieved pa<strong>in</strong> is unacceptable and<br />
if ignored it can make it more difficult <strong>for</strong> adequate pa<strong>in</strong><br />
control to be achieved. It is also important to remember that<br />
the cl<strong>in</strong>ician’s primary diagnostic tool is not pa<strong>in</strong>.<br />
When an appropriate pa<strong>in</strong> rat<strong>in</strong>g scale (e.g. 0–10) is used and<br />
the person is given sufficient time to process and respond,<br />
many cognitively impaired residents can use a pa<strong>in</strong> rat<strong>in</strong>g<br />
scale.<br />
<strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> a <strong>Palliative</strong> <strong>Approach</strong> <strong>in</strong> <strong>Residential</strong> <strong>Aged</strong> <strong>Care</strong> 73