2,46 Mb - GuÃaSalud
2,46 Mb - GuÃaSalud
2,46 Mb - GuÃaSalud
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
8.2. Insulin therapy<br />
8.2.1. Association of insulin with oral antidiabetic drugs<br />
A Cochrane (144) SR and several subsequent clinical trials (145-147) have assessed<br />
the effect of the combination of insulin with oral anti-diabetic drugs in<br />
contrast to monotherapy with insulin. All the trials assess glycemic control and<br />
the adverse effects, though they do not assess the effect on morbimortality. The<br />
guidelines and types of insulin used differ in diverse trials. In the SR (144), the<br />
combination of NPH (Neutral Protamine Hagedorn) insulin on a single night dose<br />
associated with an oral anti-diabetic drug presented a glycemic control comparable<br />
to monotherapy with human insulin (no analogues) every 12 hours or on<br />
a multiple schedule. Weight increase was much less with the night schedules of<br />
insulin associated with metformin (with or without sulfonylureas) in contrast to<br />
monotherapy with insulin (144).<br />
The results of the subsequent studies follow the same lines; in general, the<br />
association of metformin with insulin improves glycemic control (expressed in<br />
HbA 1<br />
c reduction) (1<strong>46</strong>-148), with less weight gained (145-147). The results in relation<br />
to the frequency of hypoglycaemias vary among the different studies; in the<br />
SR (144) no differences were observed as regards hypoglycaemia events, though<br />
in other studies (145; 148) the treatment combined with a dose of insulin plus<br />
metformin was associated with less hypoglycaemias in comparison with insulin<br />
taken twice on a daily basis.<br />
In the Douek (1<strong>46</strong>) study more hypoglycaemias were observed than in the<br />
group with insulin plus metformin in comparison to insulin with placebo.<br />
In general, the more intense the treatment is, the better the achievement of<br />
glycemic control and the higher the incidence of hypoglycaemia. Should there be<br />
no conclusive evidence on which guideline is better, then the patient’s preferences<br />
(79) and the risk of adverse effects, mainly hypoglycaemia, should be taken into<br />
consideration.<br />
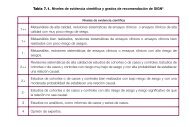
SR of RCT<br />
and RCT<br />
1+<br />
8.2.2. Insulin analogues<br />
There are many possible insulinization schedules, both as regards dosage frequency<br />
as the type of insulin: fast-acting insulin, intermediate or mixed human insulin<br />
or fast-acting analogues of human insulin (lispro, aspart and glulisine) or slowacting<br />
insulin analogues (glargine and detemir).<br />
Fast-acting insulin analogues are absorbed faster and manage to double the<br />
concentrations of insulin in plasma in half the time in comparison to human insulin,<br />
due to their pharmacokinetics. This characteristic creates lower glucose levels<br />
after the meals. Another advantage of fast-acting insulin analogues would be the<br />
possibility to inject insulin just before the meals.<br />
While fast-acting insulin analogues are used to imitate the response of eNdogenous<br />
insulin to the intake or to improve or prevent «inter-intake» hyper-<br />
70 CLINICAL PRACTICE GUIDELINES IN THE NHS