Vol 44 # 4 December 2012 - Kma.org.kw
Vol 44 # 4 December 2012 - Kma.org.kw
Vol 44 # 4 December 2012 - Kma.org.kw
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
281<br />
Asthma during Pregnancy: An Immunologic Perspective<br />
<strong>December</strong> <strong>2012</strong><br />
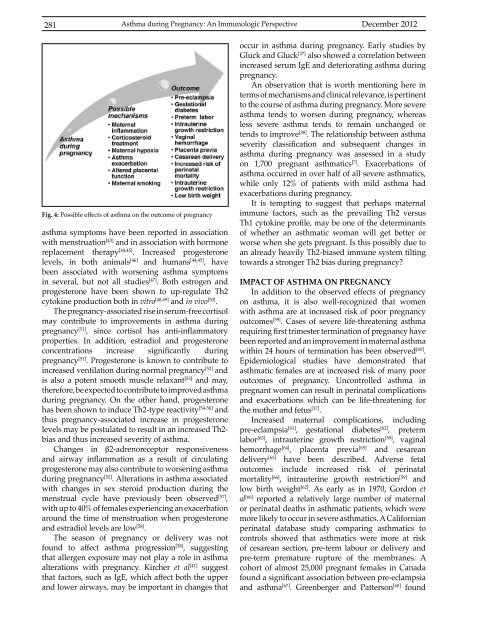
Fig. 4: Possible effects of asthma on the outcome of pregnancy<br />
asthma symptoms have been reported in association<br />
with menstruation [43] and in association with hormone<br />
replacement therapy [<strong>44</strong>,45] . Increased progesterone<br />
levels, in both animals [46] and humans [<strong>44</strong>,45] , have<br />
been associated with worsening asthma symptoms<br />
in several, but not all studies [47] . Both estrogen and<br />
progesterone have been shown to up-regulate Th2<br />
cytokine production both in vitro [48,49] and in vivo [50] .<br />
The pregnancy-associated rise in serum-free cortisol<br />
may contribute to improvements in asthma during<br />
pregnancy [51] , since cortisol has anti-inflammatory<br />
properties. In addition, estradiol and progesterone<br />
concentrations increase significantly during<br />
pregnancy [51] . Progesterone is known to contribute to<br />
increased ventilation during normal pregnancy [52] and<br />
is also a potent smooth muscle relaxant [53] and may,<br />
therefore, be expected to contribute to improved asthma<br />
during pregnancy. On the other hand, progesterone<br />
has been shown to induce Th2-type reactivity [54-56] and<br />
thus pregnancy-associated increase in progesterone<br />
levels may be postulated to result in an increased Th2-<br />
bias and thus increased severity of asthma.<br />
Changes in β2-adrenoreceptor responsiveness<br />
and airway inflammation as a result of circulating<br />
progesterone may also contribute to worsening asthma<br />
during pregnancy [52] . Alterations in asthma associated<br />
with changes in sex steroid production during the<br />
menstrual cycle have previously been observed [57] ,<br />
with up to 40% of females experiencing an exacerbation<br />
around the time of menstruation when progesterone<br />
and estradiol levels are low [58] .<br />
The season of pregnancy or delivery was not<br />
found to affect asthma progression [38] , suggesting<br />
that allergen exposure may not play a role in asthma<br />
alterations with pregnancy. Kircher et al [41] suggest<br />
that factors, such as IgE, which affect both the upper<br />
and lower airways, may be important in changes that<br />
occur in asthma during pregnancy. Early studies by<br />
Gluck and Gluck [37] also showed a correlation between<br />
increased serum IgE and deteriorating asthma during<br />
pregnancy.<br />
An observation that is worth mentioning here in<br />
terms of mechanisms and clinical relevance, is pertinent<br />
to the course of asthma during pregnancy. More severe<br />
asthma tends to worsen during pregnancy, whereas<br />
less severe asthma tends to remain unchanged or<br />
tends to improve [38] . The relationship between asthma<br />
severity classification and subsequent changes in<br />
asthma during pregnancy was assessed in a study<br />
on 1,700 pregnant asthmatics [7] . Exacerbations of<br />
asthma occurred in over half of all severe asthmatics,<br />
while only 12% of patients with mild asthma had<br />
exacerbations during pregnancy.<br />
It is tempting to suggest that perhaps maternal<br />
immune factors, such as the prevailing Th2 versus<br />
Th1 cytokine profile, may be one of the determinants<br />
of whether an asthmatic woman will get better or<br />
worse when she gets pregnant. Is this possibly due to<br />
an already heavily Th2-biased immune system tilting<br />
towards a stronger Th2 bias during pregnancy?<br />
IMPACT OF ASTHMA ON PREGNANCY<br />
In addition to the observed effects of pregnancy<br />
on asthma, it is also well-recognized that women<br />
with asthma are at increased risk of poor pregnancy<br />
outcomes [59] . Cases of severe life-threatening asthma<br />
requiring first trimester termination of pregnancy have<br />
been reported and an improvement in maternal asthma<br />
within 24 hours of termination has been observed [60] .<br />
Epidemiological studies have demonstrated that<br />
asthmatic females are at increased risk of many poor<br />
outcomes of pregnancy. Uncontrolled asthma in<br />
pregnant women can result in perinatal complications<br />
and exacerbations which can be life-threatening for<br />
the mother and fetus [37] .<br />
Increased maternal complications, including<br />
pre-eclampsia [61] , gestational diabetes [62] , preterm<br />
labor [63] , intrauterine growth restriction [59] , vaginal<br />
hemorrhage [64] , placenta previa [65] and cesarean<br />
delivery [65] have been described. Adverse fetal<br />
outcomes include increased risk of perinatal<br />
mortality [66] , intrauterine growth restriction [59] and<br />
low birth weight [62] . As early as in 1970, Gordon et<br />
al [66] reported a relatively large number of maternal<br />
or perinatal deaths in asthmatic patients, which were<br />
more likely to occur in severe asthmatics. A Californian<br />
perinatal database study comparing asthmatics to<br />
controls showed that asthmatics were more at risk<br />
of cesarean section, pre-term labour or delivery and<br />
pre-term premature rupture of the membranes. A<br />
cohort of almost 25,000 pregnant females in Canada<br />
found a significant association between pre-eclampsia<br />
and asthma [67] . Greenberger and Patterson [68] found