Vol 44 # 4 December 2012 - Kma.org.kw
Vol 44 # 4 December 2012 - Kma.org.kw
Vol 44 # 4 December 2012 - Kma.org.kw
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
293<br />
Total Hip Replacement in Nigeria: A Preliminary Report<br />
<strong>December</strong> <strong>2012</strong><br />
Table 3: Previous interventions<br />
Procedure<br />
Girdlestone excision arthroplasty<br />
Angle blade plating<br />
Hemiarthroplasty<br />
Frequency<br />
(n)<br />
2<br />
3<br />
1<br />
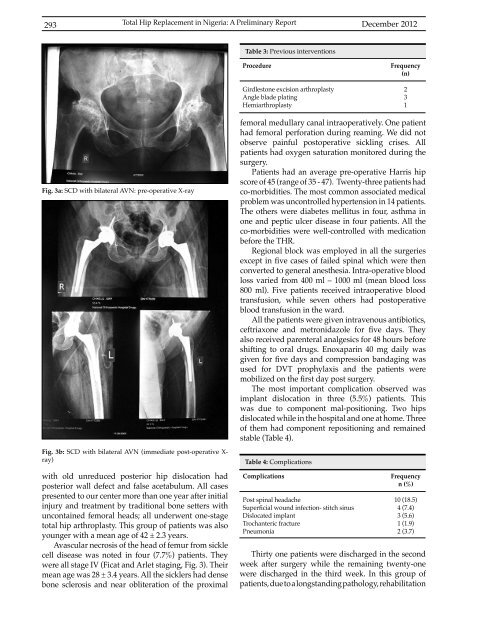
Fig. 3a: SCD with bilateral AVN: pre-operative X-ray<br />
Fig. 3b: SCD with bilateral AVN (immediate post-operative X-<br />
ray)<br />
with old unreduced posterior hip dislocation had<br />
posterior wall defect and false acetabulum. All cases<br />
presented to our center more than one year after initial<br />
injury and treatment by traditional bone setters with<br />
uncontained femoral heads; all underwent one-stage<br />
total hip arthroplasty. This group of patients was also<br />
younger with a mean age of 42 ± 2.3 years.<br />
Avascular necrosis of the head of femur from sickle<br />
cell disease was noted in four (7.7%) patients. They<br />
were all stage IV (Ficat and Arlet staging, Fig. 3). Their<br />
mean age was 28 ± 3.4 years. All the sicklers had dense<br />
bone sclerosis and near obliteration of the proximal<br />
femoral medullary canal intraoperatively. One patient<br />
had femoral perforation during reaming. We did not<br />
observe painful postoperative sickling crises. All<br />
patients had oxygen saturation monitored during the<br />
surgery.<br />
Patients had an average pre-operative Harris hip<br />
score of 45 (range of 35 - 47). Twenty-three patients had<br />
co-morbidities. The most common associated medical<br />
problem was uncontrolled hypertension in 14 patients.<br />
The others were diabetes mellitus in four, asthma in<br />
one and peptic ulcer disease in four patients. All the<br />
co-morbidities were well-controlled with medication<br />
before the THR.<br />
Regional block was employed in all the surgeries<br />
except in five cases of failed spinal which were then<br />
converted to general anesthesia. Intra-operative blood<br />
loss varied from 400 ml – 1000 ml (mean blood loss<br />
800 ml). Five patients received intraoperative blood<br />
transfusion, while seven others had postoperative<br />
blood transfusion in the ward.<br />
All the patients were given intravenous antibiotics,<br />
ceftriaxone and metronidazole for five days. They<br />
also received parenteral analgesics for 48 hours before<br />
shifting to oral drugs. Enoxaparin 40 mg daily was<br />
given for five days and compression bandaging was<br />
used for DVT prophylaxis and the patients were<br />
mobilized on the first day post surgery.<br />
The most important complication observed was<br />
implant dislocation in three (5.5%) patients. This<br />
was due to component mal-positioning. Two hips<br />
dislocated while in the hospital and one at home. Three<br />
of them had component repositioning and remained<br />
stable (Table 4).<br />
Table 4: Complications<br />
Complications<br />
Post spinal headache<br />
Superficial wound infection- stitch sinus<br />
Dislocated implant<br />
Trochanteric fracture<br />
Pneumonia<br />
Frequency<br />
n (%)<br />
10 (18.5)<br />
4 (7.4)<br />
3 (5.6)<br />
1 (1.9)<br />
2 (3.7)<br />
Thirty one patients were discharged in the second<br />
week after surgery while the remaining twenty-one<br />
were discharged in the third week. In this group of<br />
patients, due to a longstanding pathology, rehabilitation