Vol 44 # 4 December 2012 - Kma.org.kw
Vol 44 # 4 December 2012 - Kma.org.kw
Vol 44 # 4 December 2012 - Kma.org.kw
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>December</strong> <strong>2012</strong><br />
KUWAIT MEDICAL JOURNAL 306<br />
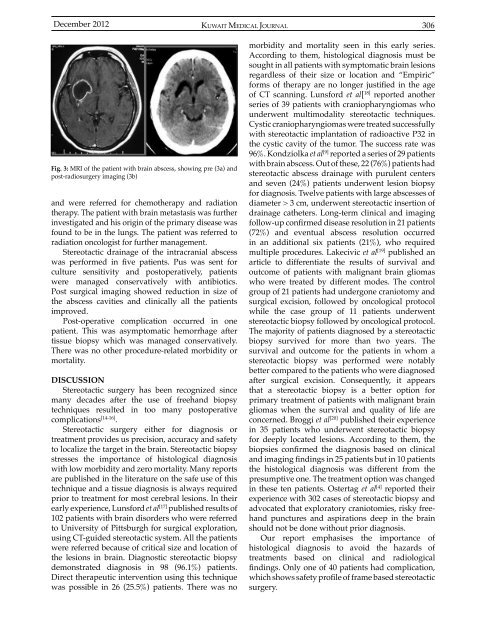
Fig. 3: MRI of the patient with brain abscess, showing pre (3a) and<br />
post-radiosurgery imaging (3b)<br />
and were referred for chemotherapy and radiation<br />
therapy. The patient with brain metastasis was further<br />
investigated and his origin of the primary disease was<br />
found to be in the lungs. The patient was referred to<br />
radiation oncologist for further management.<br />
Stereotactic drainage of the intracranial abscess<br />
was performed in five patients. Pus was sent for<br />
culture sensitivity and postoperatively, patients<br />
were managed conservatively with antibiotics.<br />
Post surgical imaging showed reduction in size of<br />
the abscess cavities and clinically all the patients<br />
improved.<br />
Post-operative complication occurred in one<br />
patient. This was asymptomatic hemorrhage after<br />
tissue biopsy which was managed conservatively.<br />
There was no other procedure-related morbidity or<br />
mortality.<br />
DISCUSSION<br />
Stereotactic surgery has been recognized since<br />
many decades after the use of freehand biopsy<br />
techniques resulted in too many postoperative<br />
complications [14-16] .<br />
Stereotactic surgery either for diagnosis or<br />
treatment provides us precision, accuracy and safety<br />
to localize the target in the brain. Stereotactic biopsy<br />
stresses the importance of histological diagnosis<br />
with low morbidity and zero mortality. Many reports<br />
are published in the literature on the safe use of this<br />
technique and a tissue diagnosis is always required<br />
prior to treatment for most cerebral lesions. In their<br />
early experience, Lunsford et al [17] published results of<br />
102 patients with brain disorders who were referred<br />
to University of Pittsburgh for surgical exploration,<br />
using CT-guided stereotactic system. All the patients<br />
were referred because of critical size and location of<br />
the lesions in brain. Diagnostic stereotactic biopsy<br />
demonstrated diagnosis in 98 (96.1%) patients.<br />
Direct therapeutic intervention using this technique<br />
was possible in 26 (25.5%) patients. There was no<br />
morbidity and mortality seen in this early series.<br />
According to them, histological diagnosis must be<br />
sought in all patients with symptomatic brain lesions<br />
regardless of their size or location and “Empiric”<br />
forms of therapy are no longer justified in the age<br />
of CT scanning. Lunsford et al[ 18] reported another<br />
series of 39 patients with craniopharyngiomas who<br />
underwent multimodality stereotactic techniques.<br />
Cystic craniopharyngiomas were treated successfully<br />
with stereotactic implantation of radioactive P32 in<br />
the cystic cavity of the tumor. The success rate was<br />
96%. Kondziolka et al [9] reported a series of 29 patients<br />
with brain abscess. Out of these, 22 (76%) patients had<br />
stereotactic abscess drainage with purulent centers<br />
and seven (24%) patients underwent lesion biopsy<br />
for diagnosis. Twelve patients with large abscesses of<br />
diameter > 3 cm, underwent stereotactic insertion of<br />
drainage catheters. Long-term clinical and imaging<br />
follow-up confirmed disease resolution in 21 patients<br />
(72%) and eventual abscess resolution occurred<br />
in an additional six patients (21%), who required<br />
multiple procedures. Lakecivic et al [19] published an<br />
article to differentiate the results of survival and<br />
outcome of patients with malignant brain gliomas<br />
who were treated by different modes. The control<br />
group of 21 patients had undergone craniotomy and<br />
surgical excision, followed by oncological protocol<br />
while the case group of 11 patients underwent<br />
stereotactic biopsy followed by oncological protocol.<br />
The majority of patients diagnosed by a stereotactic<br />
biopsy survived for more than two years. The<br />
survival and outcome for the patients in whom a<br />
stereotactic biopsy was performed were notably<br />
better compared to the patients who were diagnosed<br />
after surgical excision. Consequently, it appears<br />
that a stereotactic biopsy is a better option for<br />
primary treatment of patients with malignant brain<br />
gliomas when the survival and quality of life are<br />
concerned. Broggi et al [20] published their experience<br />
in 35 patients who underwent stereotactic biopsy<br />
for deeply located lesions. According to them, the<br />
biopsies confirmed the diagnosis based on clinical<br />
and imaging findings in 25 patients but in 10 patients<br />
the histological diagnosis was different from the<br />
presumptive one. The treatment option was changed<br />
in these ten patients. Ostertag et al [4] reported their<br />
experience with 302 cases of stereotactic biopsy and<br />
advocated that exploratory craniotomies, risky freehand<br />
punctures and aspirations deep in the brain<br />
should not be done without prior diagnosis.<br />
Our report emphasises the importance of<br />
histological diagnosis to avoid the hazards of<br />
treatments based on clinical and radiological<br />
findings. Only one of 40 patients had complication,<br />
which shows safety profile of frame based stereotactic<br />
surgery.