PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Prior Authorization<br />
Prior authorization is the utilization review processes to decide whether the requested service, procedure,<br />
medication or medical device meets clinical criteria for coverage. Prior authorization is not a guarantee of<br />
payment for care or services given to members. The prior authorization process requires the collection of<br />
information before inpatient admissions, performance of ambulatory procedures or delivery of selected services<br />
in order to:<br />
• Permit verification of eligibility and benefits<br />
• Provide a chance for communication with the doctor and/or the member<br />
• Coordinate the patient’s transition across the continuum of care<br />
• Help in the identification of members eligible for special programs<br />
A Primary Care Provider must complete the Texas Referral/ Authorization Form for all services on the <strong>Parkland</strong><br />
Prior Authorization list except for the following:<br />
• Submit all DME requests on the Title XIX form<br />
• Submit all initial outpatient therapy requests utilizing the TP1 form<br />
• Submit TP1 (request for initial outpatient therapy) or TP2 (request for extension of outpatient therapy).<br />
The completed form (Appendix D) should be faxed to the Medical Management Department at the number<br />
listed in the Important Numbers (see page 1 of this manual).<br />
Notification regarding newborn and sonogram process<br />
The authorization process for newborn delivery/admission and sonograms is as follows:<br />
Newborn admission/delivery B process:<br />
• Authorization must be requested for any newborn after day 4 of stay<br />
• DRG hospitals must meet the acute LOC level of care<br />
• A prepayment review will be conducted on all DRG 790's<br />
• All others will be paid - with random audits conducted periodically.<br />
Sonogram process:<br />
• CHIP Perinate -– Members can get one sonogram per pregnancy. For additional procedures, there must be a high- risk<br />
diagnosis along with supporting clinical documentation. Information must be submitted and approved prior to the 2nd<br />
sonogram being performed. Complete the Texas Referral Authorization Form and fax to 1-800-240-0410.<br />
OB process:<br />
• No authorization is required for OB global days (2-day uncomplicated delivery & 4-day uncomplicated C-section).<br />
• Anything outside of the OB global must be authorized.<br />
• If the DRG is a higher DRG upon submission of claim, must follow the current appeal process for any denied claims.<br />
Contact your provider relations representative or call 1-888-672-2277 with questions about these changes.<br />
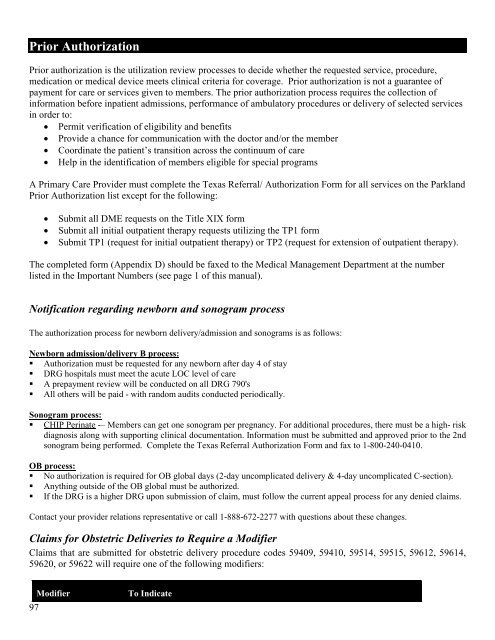
Claims for Obstetric Deliveries to Require a Modifier<br />
Claims that are submitted for obstetric delivery procedure codes 59409, 59410, 59514, 59515, 59612, 59614,<br />
59620, or 59622 will require one of the following modifiers:<br />
97<br />
Modifier<br />
To Indicate