PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
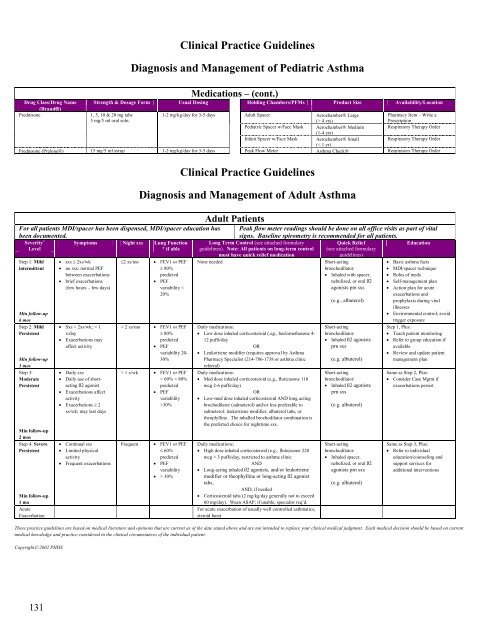
Clinical Practice Guidelines<br />
Diagnosis and Management of Pediatric Asthma<br />
Medications – (cont.)<br />
Drug Class/Drug Name Strength & Dosage Form Usual Dosing Holding Chambers/PFMs Product Size Availability/Location<br />
(Brand®)<br />
Prednisone<br />
1, 5, 10 & 20 mg tabs<br />
5 mg/5 ml oral soln.<br />
1-2 mg/kg/day for 3-5 days Adult Spacer Aerochamber® Large<br />
(> 4 yrs)<br />
Pharmacy Item – Write a<br />
Prescription<br />
Pediatric Spacer w/Face Mask Aerochamber® Medium Respiratory Therapy Order<br />
(1-4 yrs)<br />
Infant Spacer w/Face Mask Aerochamber® Small<br />
Respiratory Therapy Order<br />
(< 1 yr)<br />
Prednisone (Prelone®) 15 mg/5 ml syrup 1-2 mg/kg/day for 3-5 days Peak Flow Meter Asthma Check® Respiratory Therapy Order<br />
For all patients MDI/spacer has been dispensed, MDI/spacer education has<br />
been documented.<br />
Severity 2<br />
Symptoms Night sxs Lung Function<br />
Level<br />
* if able<br />
Step 1: Mild<br />
intermittent<br />
Min follow-up<br />
6 mos<br />
Step 2: Mild<br />
Persistent<br />
Min follow-up<br />
3 mos<br />
Step 3:<br />
Moderate<br />
Persistent<br />
Min follow-up<br />
2 mos<br />
Step 4: Severe<br />
Persistent<br />
Min follow-up<br />
1 mo<br />
Acute<br />
Exacerbation<br />
• sxs ≤ 2xs/wk<br />
• no sxs; normal PEF<br />
between exacerbations<br />
• brief exacerbations<br />
(few hours – few days)<br />
• Sxs > 2xs/wk; < 1<br />
x/day<br />
• Exacerbations may<br />
affect activity<br />
• Daily sxs<br />
• Daily use of shortacting<br />
ß2 agonist<br />
• Exacerbations affect<br />
activity<br />
• Exacerbations ≥ 2<br />
xs/wk; may last days<br />
• Continual sxs<br />
• Limited physical<br />
activity<br />
• Frequent exacerbations<br />
≤2 xs/mo<br />
Clinical Practice Guidelines<br />
Diagnosis and Management of Adult Asthma<br />
• FEV1 or PEF<br />
≥ 80%<br />
predicted<br />
• PEF<br />
variability <<br />
20%<br />
> 2 xs/mo • FEV1 or PEF<br />
≥ 80%<br />
predicted<br />
• PEF<br />
variability 20-<br />
30%<br />
> 1 x/wk • FEV1 or PEF<br />
> 60% < 80%<br />
predicted<br />
• PEF<br />
variability<br />
>30%<br />
Frequent<br />
• FEV1 or PEF<br />
≤ 60%<br />
predicted<br />
• PEF<br />
variability<br />
• > 30%<br />
Adult Patients<br />
Peak flow meter readings should be done on all office visits as part of vital<br />
signs. Baseline spirometry is recommended for all patients.<br />
Quick Relief<br />
Education<br />
(see attached formulary<br />
guidelines)<br />
Long Term Control (see attached formulary<br />
guidelines). Note: All patients on long-term control<br />
must have quick relief medication<br />
None needed<br />
Daily medications:<br />
• Low dose inhaled corticosteroid (.eg., beclomethasone 4-<br />
12 puffs/day<br />
OR<br />
• Leukotriene modifier (requires approval by Asthma<br />
Pharmacy Specialist (214-786-1738 or asthma clinic<br />
referral)<br />
Daily medications:<br />
• Med dose inhaled corticosteroid (e.g., fluticasone 110<br />
mcg 2-6 puffs/day)<br />
OR<br />
• Low-med dose inhaled corticosteroid AND long acting<br />
brochodilator (salmeterol) and/or less preferable to<br />
salmeterol: leukotriene modifier, albuterol tabs, or<br />
theoplylline. The inhalled brochodilator combination is<br />
the preferred choice for nighttime sxs.<br />
Daily medications:<br />
• High dose inhaled corticosteroid (e.g., fluticasone 220<br />
mcg > 3 puffs/day, restricted to asthma clinic<br />
AND<br />
• Long-acting inhaled ß2 agonists, and/or leukotriene<br />
modifier or theophylline or long-acting ß2 agonist<br />
tabs,<br />
AND, if needed<br />
• Corticosteroid tabs (2 mg/kg/day generally not to exceed<br />
60 mg/day). Wean ASAP; if unable, specialist req’d.<br />
For acute exacerbation of usually well controlled asthmatics,<br />
steroid burst<br />
Short-acting<br />
bronchodilator:<br />
• Inhaled with spacer,<br />
nebulized, or oral ß2<br />
agonists pm sxs<br />
(e.g., albuterol)<br />
Short-acting<br />
bronchodilator:<br />
• Inhaled ß2 agonists<br />
prn sxs<br />
(e.g. albuterol)<br />
Short-acting<br />
bronchodilator:<br />
• Inhaled ß2 agonists<br />
prn sxs<br />
(e.g. albuterol)<br />
Short-acting<br />
bronchodilator:<br />
• Inhaled spacer,<br />
nebulized, or oral ß2<br />
agonists prn sxs<br />
(e.g. albuterol)<br />
• Basic asthma facts<br />
• MDI/spacer technique<br />
• Roles of meds<br />
• Self-management plan<br />
• Action plan for acute<br />
exacerbations and<br />
prophylaxis during viral<br />
illnesses<br />
• Environmental control; avoid<br />
trigger exposure<br />
Step 1, Plus:<br />
• Teach patient monitoring<br />
• Refer to group education if<br />
available<br />
• Review and update patient<br />
management plan<br />
Same as Step 2, Plus:<br />
• Consider Case Mgmt if<br />
exacerbations persist<br />
Same as Step 3, Plus:<br />
• Refer to individual<br />
education/counseling and<br />
support services for<br />
additional interventions<br />
These practice guidelines are based on medical literature and opinions that are current as of the date stated above and are not intended to replace your clinical medical judgment. Each medical decision should be based on current<br />
medical knowledge and practice considered in the clinical circumstances of the individual patient.<br />
Copyright© 2002 PHHS<br />
131