PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
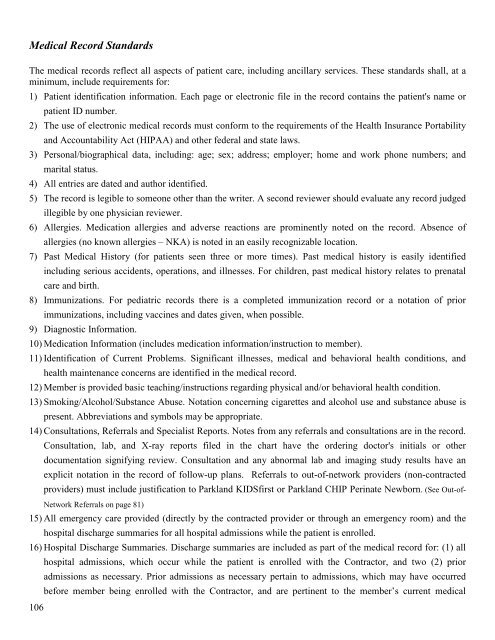
Medical Record Standards<br />
The medical records reflect all aspects of patient care, including ancillary services. These standards shall, at a<br />
minimum, include requirements for:<br />
1) Patient identification information. Each page or electronic file in the record contains the patient's name or<br />
patient ID number.<br />
2) The use of electronic medical records must conform to the requirements of the <strong>Health</strong> Insurance Portability<br />
and Accountability Act (HIPAA) and other federal and state laws.<br />
3) Personal/biographical data, including: age; sex; address; employer; home and work phone numbers; and<br />
marital status.<br />
4) All entries are dated and author identified.<br />
5) The record is legible to someone other than the writer. A second reviewer should evaluate any record judged<br />
illegible by one physician reviewer.<br />
6) Allergies. Medication allergies and adverse reactions are prominently noted on the record. Absence of<br />
allergies (no known allergies – NKA) is noted in an easily recognizable location.<br />
7) Past Medical History (for patients seen three or more times). Past medical history is easily identified<br />
including serious accidents, operations, and illnesses. For children, past medical history relates to prenatal<br />
care and birth.<br />
8) Immunizations. For pediatric records there is a completed immunization record or a notation of prior<br />
immunizations, including vaccines and dates given, when possible.<br />
9) Diagnostic Information.<br />
10) Medication Information (includes medication information/instruction to member).<br />
11) Identification of Current Problems. Significant illnesses, medical and behavioral health conditions, and<br />
health maintenance concerns are identified in the medical record.<br />
12) Member is provided basic teaching/instructions regarding physical and/or behavioral health condition.<br />
13) Smoking/Alcohol/Substance Abuse. Notation concerning cigarettes and alcohol use and substance abuse is<br />
present. Abbreviations and symbols may be appropriate.<br />
14) Consultations, Referrals and Specialist Reports. Notes from any referrals and consultations are in the record.<br />
Consultation, lab, and X-ray reports filed in the chart have the ordering doctor's initials or other<br />
documentation signifying review. Consultation and any abnormal lab and imaging study results have an<br />
explicit notation in the record of follow-up plans. Referrals to out-of-network providers (non-contracted<br />
providers) must include justification to <strong>Parkland</strong> KIDSfirst or <strong>Parkland</strong> CHIP Perinate Newborn. (See Out-of-<br />
106<br />
Network Referrals on page 81)<br />
15) All emergency care provided (directly by the contracted provider or through an emergency room) and the<br />
hospital discharge summaries for all hospital admissions while the patient is enrolled.<br />
16) Hospital Discharge Summaries. Discharge summaries are included as part of the medical record for: (1) all<br />
hospital admissions, which occur while the patient is enrolled with the Contractor, and two (2) prior<br />
admissions as necessary. Prior admissions as necessary pertain to admissions, which may have occurred<br />
before member being enrolled with the Contractor, and are pertinent to the member’s current medical