PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
PARKLAND HEALTHfirst - Parkland Community Health Plan, Inc.
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
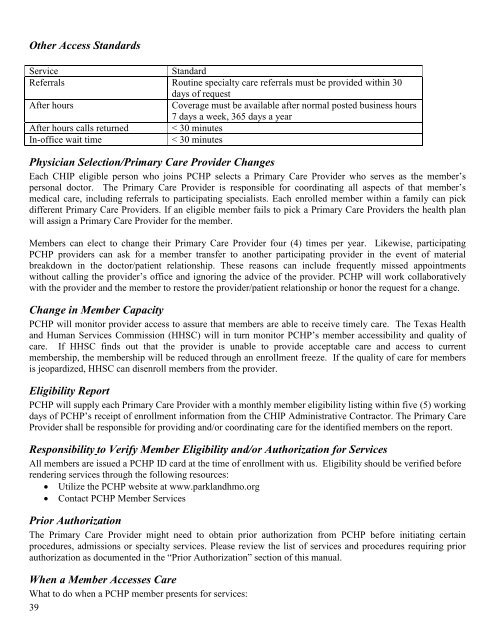
Other Access Standards<br />
Service<br />
Standard<br />
Referrals Routine specialty care referrals must be provided within 30<br />
days of request<br />
After hours<br />
Coverage must be available after normal posted business hours<br />
7 days a week, 365 days a year<br />
After hours calls returned < 30 minutes<br />
In-office wait time<br />
< 30 minutes<br />
Physician Selection/Primary Care Provider Changes<br />
Each CHIP eligible person who joins PCHP selects a Primary Care Provider who serves as the member’s<br />
personal doctor. The Primary Care Provider is responsible for coordinating all aspects of that member’s<br />
medical care, including referrals to participating specialists. Each enrolled member within a family can pick<br />
different Primary Care Providers. If an eligible member fails to pick a Primary Care Providers the health plan<br />
will assign a Primary Care Provider for the member.<br />
Members can elect to change their Primary Care Provider four (4) times per year. Likewise, participating<br />
PCHP providers can ask for a member transfer to another participating provider in the event of material<br />
breakdown in the doctor/patient relationship. These reasons can include frequently missed appointments<br />
without calling the provider’s office and ignoring the advice of the provider. PCHP will work collaboratively<br />
with the provider and the member to restore the provider/patient relationship or honor the request for a change.<br />
Change in Member Capacity<br />
PCHP will monitor provider access to assure that members are able to receive timely care. The Texas <strong>Health</strong><br />
and Human Services Commission (HHSC) will in turn monitor PCHP’s member accessibility and quality of<br />
care. If HHSC finds out that the provider is unable to provide acceptable care and access to current<br />
membership, the membership will be reduced through an enrollment freeze. If the quality of care for members<br />
is jeopardized, HHSC can disenroll members from the provider.<br />
Eligibility Report<br />
PCHP will supply each Primary Care Provider with a monthly member eligibility listing within five (5) working<br />
days of PCHP’s receipt of enrollment information from the CHIP Administrative Contractor. The Primary Care<br />
Provider shall be responsible for providing and/or coordinating care for the identified members on the report.<br />
Responsibility to Verify Member Eligibility and/or Authorization for Services<br />
All members are issued a PCHP ID card at the time of enrollment with us. Eligibility should be verified before<br />
rendering services through the following resources:<br />
• Utilize the PCHP website at www.parklandhmo.org<br />
• Contact PCHP Member Services<br />
Prior Authorization<br />
The Primary Care Provider might need to obtain prior authorization from PCHP before initiating certain<br />
procedures, admissions or specialty services. Please review the list of services and procedures requiring prior<br />
authorization as documented in the “Prior Authorization” section of this manual.<br />
When a Member Accesses Care<br />
What to do when a PCHP member presents for services:<br />
39