Neurological Examination, clinical cases and neuropsychological ...
Neurological Examination, clinical cases and neuropsychological ...
Neurological Examination, clinical cases and neuropsychological ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
23/07/54<br />
This 48‐year‐old woman had the sudden onset <strong>and</strong> rapid progression of her symptoms,<br />
which is the temporal profile of an acute vascular event or a stroke. Risk factors for stroke<br />
include hypertension, cardiac disease, diabetes mellitus, smoking as well as coagulation <strong>and</strong><br />
autoimmune disorders. This patient had none of these risk factors.<br />
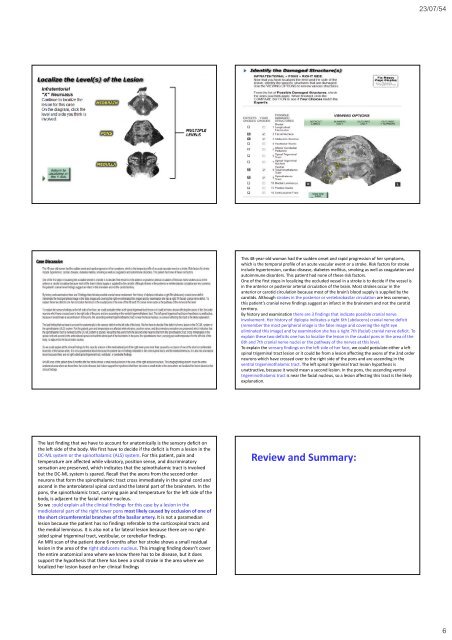
One of the first steps in localizing the occluded vessel in a stroke is to decide if the vessel is<br />
in the anterior or posterior arterial circulation of the brain. Most strokes occur in the<br />
anterior or carotid circulation because most of the brain’s blood supply is supplied by the<br />
carotids. Although strokes in the posterior or vertebrobasilar circulation are less common,<br />
this patient’s cranial nerve findings suggest an infarct in the brainstem <strong>and</strong> not the carotid<br />
territory.<br />
By history <strong>and</strong> examination there are 3 findings that indicate possible cranial nerve<br />
involvement. Her history of diplopia indicates a right 6th (abducens) cranial nerve deficit<br />
(remember the most peripheral image is the false image <strong>and</strong> covering the right eye<br />
eliminated this image) <strong>and</strong> by examination she has a right 7th (facial) cranial nerve deficit. To<br />
explain these two deficits one has to localize the lesion in the caudal pons in the area of the<br />
6th <strong>and</strong> 7th cranial nerve nuclei or the pathway of the nerves at this level.<br />
To explain the sensory findings on the left side of her face, we could postulate either a left<br />
spinal trigeminal tract lesion or it could be from a lesion affecting the axons of the 2nd order<br />
neurons which have crossed over to the right side of the pons <strong>and</strong> are ascending in the<br />
ventral trigeminothalamic tract. The left spinal trigeminal tract lesion hypothesis is<br />
unattractive, because it would mean a second lesion. In the pons, the ascending ventral<br />
trigeminothalamic tract is near the facial nucleus, so a lesion affecting this tract is the likely<br />
explanation.<br />
The last finding that we have to account for anatomically is the sensory deficit on<br />
the left side of the body. We first have to decide if the deficit is from a lesion in the<br />
DC‐ML system or the spinothalamic (ALS) system. For this patient, pain <strong>and</strong><br />
temperature are affected while vibratory, position sense, <strong>and</strong> discriminatory<br />
sensation are preserved, which indicates that the spinothalamic tract is involved<br />
but the DC‐ML system is spared. Recall that the axons from the second order<br />
neurons that form the spinothalamic tract cross immediately in the spinal cord <strong>and</strong><br />
ascend in the anterolateral spinal cord <strong>and</strong> the lateral part of the brainstem. In the<br />
pons, the spinothalamic tract, carrying pain <strong>and</strong> temperature for the left side of the<br />
body, is adjacent to the facial motor nucleus.<br />
So we could explain all the <strong>clinical</strong> findings for this case by a lesion in the<br />
mediolateral part of the right lower pons most likely caused by occlusion of one of<br />
the short circumferential branches of the basilar artery. It is not a paramedian<br />
lesion because the patient has no findings referable to the corticospinal tracts <strong>and</strong><br />
the medial lemniscus. It is also not a far lateral lesion because there are no rightsided<br />
spinal trigeminal tract, vestibular, or cerebellar findings.<br />
An MRI scan of the patient done 6 months after her stroke shows a small residual<br />
lesion in the area of the right abducens nucleus. This imaging finding doesn’t cover<br />
the entire anatomical area where we know there has to be disease, but it does<br />
support the hypothesis that there has been a small stroke in the area where we<br />
localized her lesion based on her <strong>clinical</strong> findings<br />
Review <strong>and</strong> Summary:<br />
6