annals 1-2.qxd - Centrum Zdrowia Dziecka
annals 1-2.qxd - Centrum Zdrowia Dziecka
annals 1-2.qxd - Centrum Zdrowia Dziecka
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
39<br />
Results<br />
Morphological changes and cytokeratin expression<br />
in the liver<br />
The frequency of histological changes is demonstrated in Table<br />
2. We have found fibrosis, inflammatory changes in the<br />
portal tracts and lobules, cholestasis in zone 3, bile ductular<br />
proliferation with abnormal structures (concentric, tubular,<br />
reduplicated), cholangiolitis in all cases, but the intensity of<br />
these changes was different (Table 3).<br />
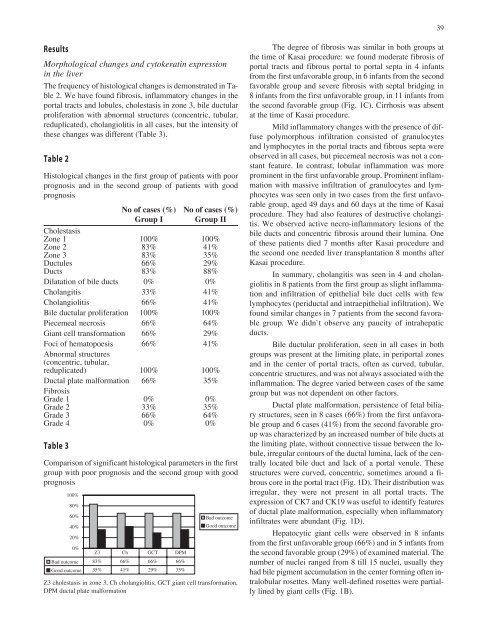
Table 2<br />
Histological changes in the first group of patients with poor<br />
prognosis and in the second group of patients with good<br />
prognosis<br />
No of cases (%) No of cases (%)<br />
Group I Group II<br />
Cholestasis<br />
Zone 1 100% 100%<br />
Zone 2 83% 41%<br />
Zone 3 83% 35%<br />
Ductules 66% 29%<br />
Ducts 83% 88%<br />
Dilatation of bile ducts 0% 0%<br />
Cholangitis 33% 41%<br />
Cholangiolitis 66% 41%<br />
Bile ductular proliferation 100% 100%<br />
Piecemeal necrosis 66% 64%<br />
Giant cell transformation 66% 29%<br />
Foci of hematopoesis 66% 41%<br />
Abnormal structures<br />
(concentric, tubular,<br />
reduplicated) 100% 100%<br />
Ductal plate malformation 66% 35%<br />
Fibrosis<br />
Grade 1 0% 0%<br />
Grade 2 33% 35%<br />
Grade 3 66% 64%<br />
Grade 4 0% 0%<br />
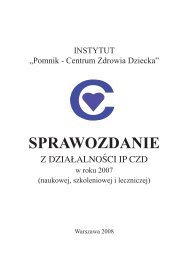
Table 3<br />
Comparison of significant histological parameters in the first<br />
group with poor prognosis and the second group with good<br />
prognosis<br />
Z3 cholestasis in zone 3, Ch cholangiolitis, GCT giant cell transformation,<br />
DPM ductal plate malformation<br />
The degree of fibrosis was similar in both groups at<br />
the time of Kasai procedure: we found moderate fibrosis of<br />
portal tracts and fibrous portal to portal septa in 4 infants<br />
from the first unfavorable group, in 6 infants from the second<br />
favorable group and severe fibrosis with septal bridging in<br />
8 infants from the first unfavorable group, in 11 infants from<br />
the second favorable group (Fig. 1C). Cirrhosis was absent<br />
at the time of Kasai procedure.<br />
Mild inflammatory changes with the presence of diffuse<br />
polymorphous infiltration consisted of granulocytes<br />
and lymphocytes in the portal tracts and fibrous septa were<br />
observed in all cases, but piecemeal necrosis was not a constant<br />
feature. In contrast, lobular inflammation was more<br />
prominent in the first unfavorable group. Prominent inflammation<br />
with massive infiltration of granulocytes and lymphocytes<br />
was seen only in two cases from the first unfavorable<br />
group, aged 49 days and 60 days at the time of Kasai<br />
procedure. They had also features of destructive cholangitis.<br />
We observed active necro-inflammatory lesions of the<br />
bile ducts and concentric fibrosis around their lumina. One<br />
of these patients died 7 months after Kasai procedure and<br />
the second one needed liver transplantation 8 months after<br />
Kasai procedure.<br />
In summary, cholangitis was seen in 4 and cholangiolitis<br />
in 8 patients from the first group as slight inflammation<br />
and infiltration of epithelial bile duct cells with few<br />
lymphocytes (periductal and intraepithelial infiltration). We<br />
found similar changes in 7 patients from the second favorable<br />
group. We didn`t observe any paucity of intrahepatic<br />
ducts.<br />
Bile ductular proliferation, seen in all cases in both<br />
groups was present at the limiting plate, in periportal zones<br />
and in the center of portal tracts, often as curved, tubular,<br />
concentric structures, and was not always associated with the<br />
inflammation. The degree varied between cases of the same<br />
group but was not dependent on other factors.<br />
Ductal plate malformation, persistence of fetal biliary<br />
structures, seen in 8 cases (66%) from the first unfavorable<br />
group and 6 cases (41%) from the second favorable group<br />
was characterized by an increased number of bile ducts at<br />
the limiting plate, without connective tissue between the lobule,<br />
irregular contours of the ductal lumina, lack of the centrally<br />
located bile duct and lack of a portal venule. These<br />
structures were curved, concentric, sometimes around a fibrous<br />
core in the portal tract (Fig. 1D). Their distribution was<br />
irregular, they were not present in all portal tracts. The<br />
expression of CK7 and CK19 was useful to identify features<br />
of ductal plate malformation, especially when inflammatory<br />
infiltrates were abundant (Fig. 1D).<br />
Hepatocytic giant cells were observed in 8 infants<br />
from the first unfavorable group (66%) and in 5 infants from<br />
the second favorable group (29%) of examined material. The<br />
number of nuclei ranged from 8 till 15 nuclei, usually they<br />
had bile pigment accumulation in the center forming often intralobular<br />
rosettes. Many well-defined rosettes were partially<br />
lined by giant cells (Fig. 1B).