Smoking and mental health - NCSCT
Smoking and mental health - NCSCT
Smoking and mental health - NCSCT
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
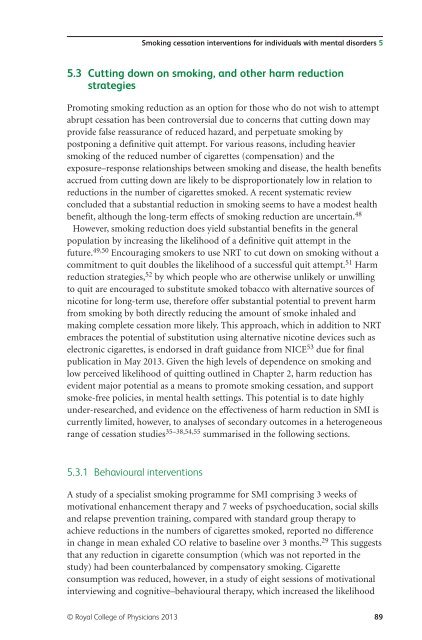
<strong>Smoking</strong> cessation interventions for individuals with <strong>mental</strong> disorders 5<br />
5.3 Cutting down on smoking, <strong>and</strong> other harm reduction<br />
strategies<br />
Promoting smoking reduction as an option for those who do not wish to attempt<br />
abrupt cessation has been controversial due to concerns that cutting down may<br />
provide false reassurance of reduced hazard, <strong>and</strong> perpetuate smoking by<br />
postponing a definitive quit attempt. For various reasons, including heavier<br />
smoking of the reduced number of cigarettes (compensation) <strong>and</strong> the<br />
exposure–response relationships between smoking <strong>and</strong> disease, the <strong>health</strong> benefits<br />
accrued from cutting down are likely to be disproportionately low in relation to<br />
reductions in the number of cigarettes smoked. A recent systematic review<br />
concluded that a substantial reduction in smoking seems to have a modest <strong>health</strong><br />
benefit, although the long-term effects of smoking reduction are uncertain. 48<br />
However, smoking reduction does yield substantial benefits in the general<br />
population by increasing the likelihood of a definitive quit attempt in the<br />
future. 49,50 Encouraging smokers to use NRT to cut down on smoking without a<br />
commitment to quit doubles the likelihood of a successful quit attempt. 51 Harm<br />
reduction strategies, 52 by which people who are otherwise unlikely or unwilling<br />
to quit are encouraged to substitute smoked tobacco with alternative sources of<br />
nicotine for long-term use, therefore offer substantial potential to prevent harm<br />
from smoking by both directly reducing the amount of smoke inhaled <strong>and</strong><br />
making complete cessation more likely. This approach, which in addition to NRT<br />
embraces the potential of substitution using alternative nicotine devices such as<br />
electronic cigarettes, is endorsed in draft guidance from NICE 53 due for final<br />
publication in May 2013. Given the high levels of dependence on smoking <strong>and</strong><br />
low perceived likelihood of quitting outlined in Chapter 2, harm reduction has<br />
evident major potential as a means to promote smoking cessation, <strong>and</strong> support<br />
smoke-free policies, in <strong>mental</strong> <strong>health</strong> settings. This potential is to date highly<br />
under-researched, <strong>and</strong> evidence on the effectiveness of harm reduction in SMI is<br />
currently limited, however, to analyses of secondary outcomes in a heterogeneous<br />
range of cessation studies 35–38,54,55 summarised in the following sections.<br />
5.3.1 Behavioural interventions<br />
A study of a specialist smoking programme for SMI comprising 3 weeks of<br />
motivational enhancement therapy <strong>and</strong> 7 weeks of psychoeducation, social skills<br />
<strong>and</strong> relapse prevention training, compared with st<strong>and</strong>ard group therapy to<br />
achieve reductions in the numbers of cigarettes smoked, reported no difference<br />
in change in mean exhaled CO relative to baseline over 3 months. 29 This suggests<br />
that any reduction in cigarette consumption (which was not reported in the<br />
study) had been counterbalanced by compensatory smoking. Cigarette<br />
consumption was reduced, however, in a study of eight sessions of motivational<br />
interviewing <strong>and</strong> cognitive–behavioural therapy, which increased the likelihood<br />
© Royal College of Physicians 2013 89