Smoking and mental health - NCSCT
Smoking and mental health - NCSCT
Smoking and mental health - NCSCT
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
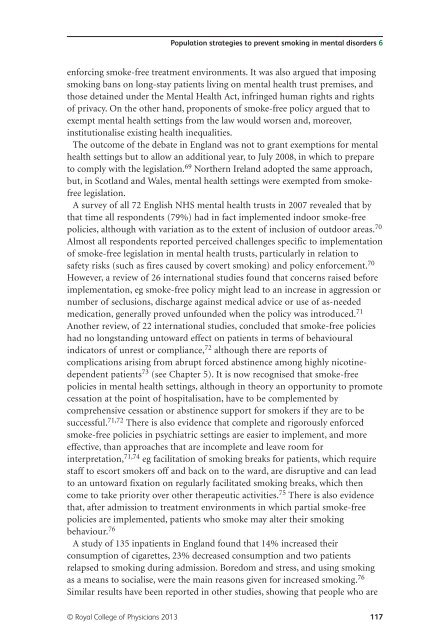
Population strategies to prevent smoking in <strong>mental</strong> disorders 6<br />
enforcing smoke-free treatment environments. It was also argued that imposing<br />
smoking bans on long-stay patients living on <strong>mental</strong> <strong>health</strong> trust premises, <strong>and</strong><br />
those detained under the Mental Health Act, infringed human rights <strong>and</strong> rights<br />
of privacy. On the other h<strong>and</strong>, proponents of smoke-free policy argued that to<br />
exempt <strong>mental</strong> <strong>health</strong> settings from the law would worsen <strong>and</strong>, moreover,<br />
institutionalise existing <strong>health</strong> inequalities.<br />
The outcome of the debate in Engl<strong>and</strong> was not to grant exemptions for <strong>mental</strong><br />
<strong>health</strong> settings but to allow an additional year, to July 2008, in which to prepare<br />
to comply with the legislation. 69 Northern Irel<strong>and</strong> adopted the same approach,<br />
but, in Scotl<strong>and</strong> <strong>and</strong> Wales, <strong>mental</strong> <strong>health</strong> settings were exempted from smokefree<br />
legislation.<br />
A survey of all 72 English NHS <strong>mental</strong> <strong>health</strong> trusts in 2007 revealed that by<br />
that time all respondents (79%) had in fact implemented indoor smoke-free<br />
policies, although with variation as to the extent of inclusion of outdoor areas. 70<br />
Almost all respondents reported perceived challenges specific to implementation<br />
of smoke-free legislation in <strong>mental</strong> <strong>health</strong> trusts, particularly in relation to<br />
safety risks (such as fires caused by covert smoking) <strong>and</strong> policy enforcement. 70<br />
However, a review of 26 international studies found that concerns raised before<br />
implementation, eg smoke-free policy might lead to an increase in aggression or<br />
number of seclusions, discharge against medical advice or use of as-needed<br />
medication, generally proved unfounded when the policy was introduced. 71<br />
Another review, of 22 international studies, concluded that smoke-free policies<br />
had no longst<strong>and</strong>ing untoward effect on patients in terms of behavioural<br />
indicators of unrest or compliance, 72 although there are reports of<br />
complications arising from abrupt forced abstinence among highly nicotinedependent<br />
patients 73 (see Chapter 5). It is now recognised that smoke-free<br />
policies in <strong>mental</strong> <strong>health</strong> settings, although in theory an opportunity to promote<br />
cessation at the point of hospitalisation, have to be complemented by<br />
comprehensive cessation or abstinence support for smokers if they are to be<br />
successful. 71,72 There is also evidence that complete <strong>and</strong> rigorously enforced<br />
smoke-free policies in psychiatric settings are easier to implement, <strong>and</strong> more<br />
effective, than approaches that are incomplete <strong>and</strong> leave room for<br />
interpretation, 71,74 eg facilitation of smoking breaks for patients, which require<br />
staff to escort smokers off <strong>and</strong> back on to the ward, are disruptive <strong>and</strong> can lead<br />
to an untoward fixation on regularly facilitated smoking breaks, which then<br />
come to take priority over other therapeutic activities. 75 There is also evidence<br />
that, after admission to treatment environments in which partial smoke-free<br />
policies are implemented, patients who smoke may alter their smoking<br />
behaviour. 76<br />
A study of 135 inpatients in Engl<strong>and</strong> found that 14% increased their<br />
consumption of cigarettes, 23% decreased consumption <strong>and</strong> two patients<br />
relapsed to smoking during admission. Boredom <strong>and</strong> stress, <strong>and</strong> using smoking<br />
as a means to socialise, were the main reasons given for increased smoking. 76<br />
Similar results have been reported in other studies, showing that people who are<br />
© Royal College of Physicians 2013 117