Smoking and mental health - NCSCT
Smoking and mental health - NCSCT
Smoking and mental health - NCSCT
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
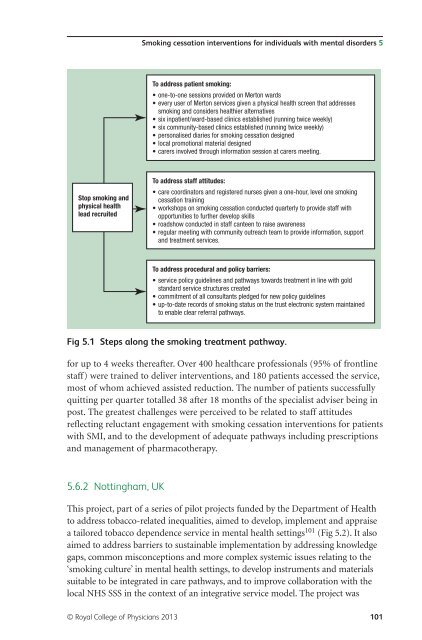
<strong>Smoking</strong> cessation interventions for individuals with <strong>mental</strong> disorders 5<br />
To address patient smoking:<br />
• one-to-one sessions provided on Merton wards<br />
• every user of Merton services given a physical <strong>health</strong> screen that addresses<br />
smoking <strong>and</strong> considers <strong>health</strong>ier alternatives<br />
• six inpatient/ward-based clinics established (running twice weekly)<br />
• six community-based clinics established (running twice weekly)<br />
• personalised diaries for smoking cessation designed<br />
• local promotional material designed<br />
• carers involved through information session at carers meeting.<br />
Stop smoking <strong>and</strong><br />
physical <strong>health</strong><br />
lead recruited<br />
To address staff attitudes:<br />
• care coordinators <strong>and</strong> registered nurses given a one-hour, level one smoking<br />
cessation training<br />
• workshops on smoking cessation conducted quarterly to provide staff with<br />
opportunities to further develop skills<br />
• roadshow conducted in staff canteen to raise awareness<br />
• regular meeting with community outreach team to provide information, support<br />
<strong>and</strong> treatment services.<br />
To address procedural <strong>and</strong> policy barriers:<br />
• service policy guidelines <strong>and</strong> pathways towards treatment in line with gold<br />
st<strong>and</strong>ard service structures created<br />
• commitment of all consultants pledged for new policy guidelines<br />
• up-to-date records of smoking status on the trust electronic system maintained<br />
to enable clear referral pathways.<br />
Fig 5.1 Steps along the smoking treatment pathway.<br />
for up to 4 weeks thereafter. Over 400 <strong>health</strong>care professionals (95% of frontline<br />
staff) were trained to deliver interventions, <strong>and</strong> 180 patients accessed the service,<br />
most of whom achieved assisted reduction. The number of patients successfully<br />
quitting per quarter totalled 38 after 18 months of the specialist adviser being in<br />
post. The greatest challenges were perceived to be related to staff attitudes<br />
reflecting reluctant engagement with smoking cessation interventions for patients<br />
with SMI, <strong>and</strong> to the development of adequate pathways including prescriptions<br />
<strong>and</strong> management of pharmacotherapy.<br />
5.6.2 Nottingham, UK<br />
This project, part of a series of pilot projects funded by the Department of Health<br />
to address tobacco-related inequalities, aimed to develop, implement <strong>and</strong> appraise<br />
a tailored tobacco dependence service in <strong>mental</strong> <strong>health</strong> settings 101 (Fig 5.2). It also<br />
aimed to address barriers to sustainable implementation by addressing knowledge<br />
gaps, common misconceptions <strong>and</strong> more complex systemic issues relating to the<br />
‘smoking culture’ in <strong>mental</strong> <strong>health</strong> settings, to develop instruments <strong>and</strong> materials<br />
suitable to be integrated in care pathways, <strong>and</strong> to improve collaboration with the<br />
local NHS SSS in the context of an integrative service model. The project was<br />
© Royal College of Physicians 2013 101