100% Positive Material Identification
23mhiW2
23mhiW2
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Editorial<br />
Understanding Implants in<br />
Knee and Hip Replacement<br />
An interview with<br />
Douglas E. Padgett, MD<br />
Chief of the Adult Reconstruction and Joint<br />
Replacement Division, Orthopedic Surgeon,<br />
Hospital for Special Surgery<br />
Information about knee and hip<br />
replacements is more easily available<br />
than ever before. But direct-toconsumer<br />
advertising, online articles and<br />
other reports in the media may make<br />
it more difficult for people considering<br />
these surgeries to understand their<br />
options. Becoming familiar with the key<br />
considerations that go into selection of<br />
the implant that is used to replace the<br />
injured or damaged joint can make the<br />
process easier.<br />
I<br />
Russell E. Windsor, MD, PC<br />
Orthopaedic Surgeon, Hospital for Special Surgery<br />
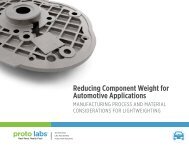
Figures 2a and b: Picture of Implant in Knee<br />
Figure 2c: X-ray<br />
of a Total Knee<br />
Arthroplasty<br />
Types of Knee Replacement<br />
In the majority of total knee<br />
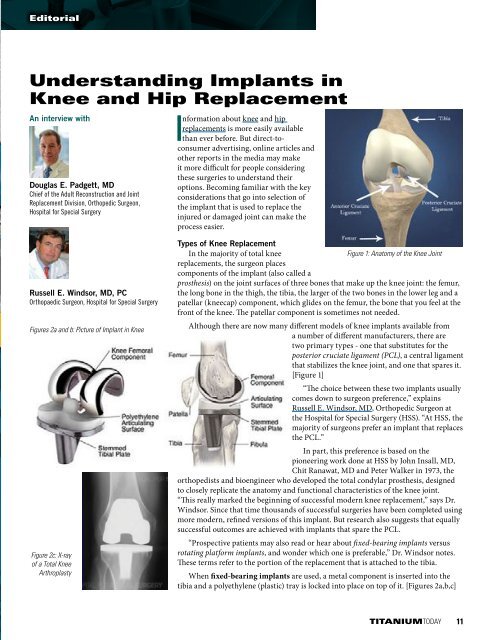
Figure 1: Anatomy of the Knee Joint<br />
replacements, the surgeon places<br />
components of the implant (also called a<br />
prosthesis) on the joint surfaces of three bones that make up the knee joint: the femur,<br />
the long bone in the thigh, the tibia, the larger of the two bones in the lower leg and a<br />
patellar (kneecap) component, which glides on the femur, the bone that you feel at the<br />
front of the knee. The patellar component is sometimes not needed.<br />
Although there are now many different models of knee implants available from<br />
a number of different manufacturers, there are<br />
two primary types - one that substitutes for the<br />
posterior cruciate ligament (PCL), a central ligament<br />
that stabilizes the knee joint, and one that spares it.<br />
[Figure 1]<br />
“The choice between these two implants usually<br />
comes down to surgeon preference,” explains<br />
Russell E. Windsor, MD, Orthopedic Surgeon at<br />
the Hospital for Special Surgery (HSS). “At HSS, the<br />
majority of surgeons prefer an implant that replaces<br />
the PCL.”<br />
In part, this preference is based on the<br />
pioneering work done at HSS by John Insall, MD,<br />
Chit Ranawat, MD and Peter Walker in 1973, the<br />
orthopedists and bioengineer who developed the total condylar prosthesis, designed<br />
to closely replicate the anatomy and functional characteristics of the knee joint.<br />
“This really marked the beginning of successful modern knee replacement,” says Dr.<br />
Windsor. Since that time thousands of successful surgeries have been completed using<br />
more modern, refined versions of this implant. But research also suggests that equally<br />
successful outcomes are achieved with implants that spare the PCL.<br />
“Prospective patients may also read or hear about fixed-bearing implants versus<br />
rotating platform implants, and wonder which one is preferable,” Dr. Windsor notes.<br />
These terms refer to the portion of the replacement that is attached to the tibia.<br />
When fixed-bearing implants are used, a metal component is inserted into the<br />
tibia and a polyethylene (plastic) tray is locked into place on top of it. [Figures 2a,b,c]<br />
TITANIUMTODAY 11