2017 HCHB_digital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
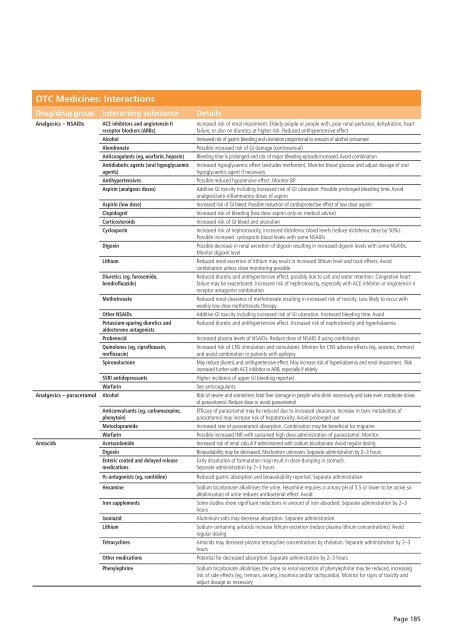
OTC Medicines: Interactions<br />
Drug/drug group Interacting substance Details<br />
Analgesics – NSAIDs<br />
ACE inhibitors and angiotensin II<br />
receptor blockers (ARBs)<br />
Alcohol<br />
Alendronate<br />
Anticoagulants (eg, warfarin, heparin)<br />
Antidiabetic agents (oral hypoglycaemic<br />
agents)<br />
Antihypertensives<br />
Aspirin (analgesic doses)<br />
Aspirin (low dose)<br />
Clopidogrel<br />
Corticosteroids<br />
Increased risk of renal impairment. Elderly people or people with, poor renal perfusion, dehydration, heart<br />
failure, or also on diuretics at higher risk. Reduced antihypertensive effect<br />
Increased risk of gastric bleeding and ulceration proportional to amount of alcohol consumed<br />
Possible increased risk of GI damage (controversial)<br />
Bleeding time is prolonged and risk of major bleeding episode increased. Avoid combination<br />
Increased hypoglycaemic effect (excludes metformin). Monitor blood glucose and adjust dosage of oral<br />
hypoglycaemic agent if necessary<br />
Possible reduced hypotensive effect. Monitor BP<br />
Additive GI toxicity including increased risk of GI ulceration. Possible prolonged bleeding time. Avoid<br />
analgesic/anti-inflammatory doses of aspirin<br />
Increased risk of GI bleed. Possible reduction of cardioprotective effect of low dose aspirin<br />
Increased risk of bleeding (low dose aspirin only on medical advice)<br />
Increased risk of GI bleed and ulceration<br />
Cyclosporin Increased risk of nephrotoxicity, increased diclofenac blood levels (reduce diclofenac dose by 50%).<br />
Possible increased cyclosporin blood levels with some NSAIDs<br />
Digoxin<br />
Possible decrease in renal excretion of digoxin resulting in increased digoxin levels with some NSAIDs.<br />
Monitor digoxin level<br />
Lithium<br />
Reduced renal excretion of lithium may result in increased lithium level and toxic effects. Avoid<br />
combination unless close monitoring possible<br />
Diuretics (eg, furosemide,<br />
bendrofluazide)<br />
Methotrexate<br />
Other NSAIDs<br />
Potassium-sparing diuretics and<br />
aldosterone antagonists<br />
Probenecid<br />
Quinolones (eg, ciprofloxacin,<br />
norfloxacin)<br />
Spironolactone<br />
SSRI antidepressants<br />
Warfarin<br />
Reduced diuretic and antihypertensive effect, possibly due to salt and water retention. Congestive heart<br />
failure may be exacerbated. Increased risk of nephrotoxicity, especially with ACE inhibitor or angiotensin II<br />
receptor antagonist combination<br />
Reduced renal clearance of methotrexate resulting in increased risk of toxicity. Less likely to occur with<br />
weekly low dose methotrexate therapy<br />
Additive GI toxicity including increased risk of GI ulceration. Increased bleeding time. Avoid<br />
Reduced diuretic and antihypertensive effect. Increased risk of nephrotoxicity and hyperkalaemia<br />
Increased plasma levels of NSAIDs. Reduce dose of NSAID if using combination<br />
Increased risk of CNS stimulation and convulsions. Monitor for CNS adverse effects (eg, seizures, tremors)<br />
and avoid combination in patients with epilepsy<br />
May reduce diuretic and antihypertensive effect. May increase risk of hyper kalaemia and renal impairment. Risk<br />
increased further with ACE inhibitor or ARB, especially if elderly<br />
Higher incidence of upper GI bleeding reported<br />
See anticoagulants<br />
Analgesics – paracetamol Alcohol Risk of severe and sometimes fatal liver damage in people who drink excessively and take even moderate doses<br />
of paracetamol. Reduce dose or avoid paracetamol<br />
Anticonvulsants (eg, carbamazepine,<br />
phenytoin)<br />
Metoclopramide<br />
Warfarin<br />
Efficacy of paracetamol may be reduced due to increased clearance. Increase in toxic metabolites of<br />
paracetamol may increase risk of hepatotoxicity. Avoid prolonged use<br />
Increased rate of paracetamol absorption. Combination may be beneficial for migraine<br />
Possible increased INR with sustained high dose administration of paracetamol. Monitor<br />
Antacids Acetazolamide Increased risk of renal calculi if administered with sodium bicarbonate. Avoid regular dosing<br />
Digoxin<br />
Bioavailability may be decreased. Mechanism unknown. Separate administration by 2–3 hours<br />
Enteric coated and delayed release<br />
medications<br />
H2-antagonists (eg, ranitidine)<br />
Early dissolution of formulation may result in dose-dumping in stomach.<br />
Separate administration by 2–3 hours<br />
Reduced gastric absorption and bioavailability reported. Separate administration<br />
Hexamine<br />
Sodium bicarbonate alkalinises the urine. Hexamine requires a urinary pH of 5.5 or lower to be active so<br />
alkalinisation of urine reduces antibacterial effect. Avoid<br />
Iron supplements Some studies show significant reductions in amount of iron absorbed. Separate administration by 2–3<br />
hours<br />
Isoniazid<br />
Aluminium salts may decrease absorption. Separate administration<br />
Lithium<br />
Sodium-containing antacids increase lithium excretion (reduce plasma lithium concentrations). Avoid<br />
regular dosing<br />
Tetracyclines Antacids may decrease plasma tetracycline concentrations by chelation. Separate administration by 2–3<br />
hours<br />
Other medications<br />
Potential for decreased absorption. Separate administration by 2–3 hours<br />
Phenylephrine<br />
Sodium bicarbonate alkalinises the urine so renal excretion of phenylephrine may be reduced, increasing<br />
risk of side effects (eg, tremors, anxiety, insomnia and/or tachycardia). Monitor for signs of toxicity and<br />
adjust dosage as necessary<br />
Page 185