2017 HCHB_digital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Asthma and COPD<br />
Asthma<br />
New Zealand has one of the highest prevalences of asthma in the world and over<br />
460,000 people regularly take medication for asthma. An estimated one in seven<br />
children and one in nine adults are affected, and only a small number of children<br />
appear to grow out of the condition.<br />
Common symptoms include wheezing (a whistling sound most obvious when<br />
breathing out), shortness of breath, tightness in the chest, difficulty speaking, and<br />
a persistent dry cough (usually at night or after exercise). Over time this cough may<br />
become more productive. A cough may be the only symptom in young children.<br />
These symptoms may occur suddenly as an asthma “attack”, or they can be<br />
present most of the time. During an “attack”, breathing becomes very difficult<br />
due to inflammation and contraction of the smooth muscle within the airway,<br />
excessive mucous secretion, and swelling of the smaller airways. Permanent<br />
damage of the airways can result from untreated asthma.<br />
It is common for asthmatics to also suffer from hay fever or eczema, and/or to<br />
have a family history of these conditions.<br />
The cause of asthma is unknown; however, many common triggers have been<br />
identified, including animal dander (especially cats), cigarette smoke, cold air,<br />
exercise, house dust mites, pollen, stress, strong perfume, viral infections (eg, a<br />
cold) and some medicines (eg, aspirin and NSAIDs). Asthma cannot be cured but<br />
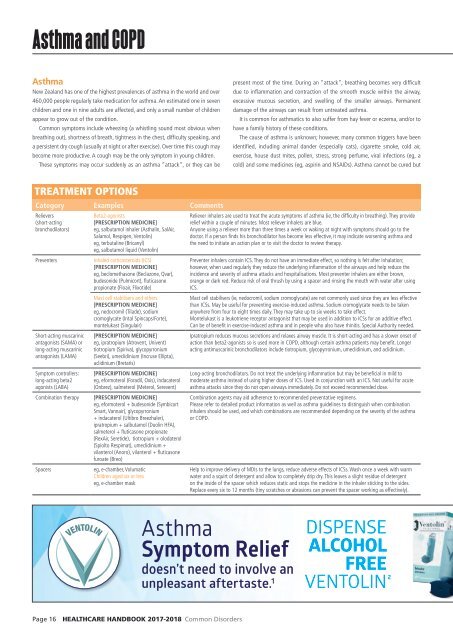
TREATMENT OPTIONS<br />
Category Examples Comments<br />
Relievers<br />
(short-acting<br />
bronchodilators)<br />
Preventers<br />
Short-acting muscarinic<br />
antagonists (SAMA) or<br />
long-acting muscarinic<br />
antagonists (LAMA)<br />
Symptom controllers:<br />
long-acting beta2<br />
agonists (LABA)<br />
Combination therapy<br />
Spacers<br />
Beta2-agonists<br />
[PRESCRIPTION MEDICINE]<br />
eg, salbutamol inhaler (Asthalin, SalAir,<br />
Salamol, Respigen, Ventolin)<br />
eg, terbutaline (Bricanyl)<br />
eg, salbutamol liquid (Ventolin)<br />
Inhaled corticosteroids (ICS)<br />
[PRESCRIPTION MEDICINE]<br />
eg, beclomethasone (Beclazone, Qvar),<br />
budesonide (Pulmicort), fluticasone<br />
propionate (Floair, Flixotide)<br />
Mast cell stabilisers and others<br />
[PRESCRIPTION MEDICINE]<br />
eg, nedocromil (Tilade), sodium<br />
cromoglycate (Intal Spincaps/Forte),<br />
montelukast (Singulair)<br />
[PRESCRIPTION MEDICINE]<br />
eg, ipratropium (Atrovent, Univent)<br />
tiotropium (Spiriva), glycopyrronium<br />
(Seebri), umeclidinium (Incruse Ellipta),<br />
aclidinium (Bretaris)<br />
[PRESCRIPTION MEDICINE]<br />
eg, eformoterol (Foradil, Oxis), indacaterol<br />
(Onbrez), salmeterol (Meterol, Serevent)<br />
[PRESCRIPTION MEDICINE]<br />
eg, eformoterol + budesonide (Symbicort<br />
Smart, Vannair), glycopyrronium<br />
+ indacaterol (Ultibro Breezhaler),<br />
ipratropium + salbutamol (Duolin HFA),<br />
salmeterol + fluticasone propionate<br />
(RexAir, Seretide), tiotropium + olodaterol<br />
(Spiolto Respimat), umeclidinium +<br />
vilanterol (Anoro), vilanterol + fluticasone<br />
furoate (Breo)<br />
eg, e-chamber, Volumatic<br />
Children aged six or less<br />
eg, e-chamber mask<br />
Reliever inhalers are used to treat the acute symptoms of asthma (ie, the difficulty in breathing). They provide<br />
relief within a couple of minutes. Most reliever inhalers are blue.<br />
Anyone using a reliever more than three times a week or waking at night with symptoms should go to the<br />
doctor. If a person finds his bronchodilator has become less effective, it may indicate worsening asthma and<br />
the need to initiate an action plan or to visit the doctor to review therapy.<br />
Preventer inhalers contain ICS. They do not have an immediate effect, so nothing is felt after inhalation;<br />
however, when used regularly they reduce the underlying inflammation of the airways and help reduce the<br />
incidence and severity of asthma attacks and hospitalisations. Most preventer inhalers are either brown,<br />
orange or dark red. Reduce risk of oral thrush by using a spacer and rinsing the mouth with water after using<br />
ICS.<br />
Mast cell stabilisers (ie, nedocromil, sodium cromoglycate) are not commonly used since they are less effective<br />
than ICSs. May be useful for preventing exercise-induced asthma. Sodium cromoglycate needs to be taken<br />
anywhere from four to eight times daily. They may take up to six weeks to take effect.<br />
Montelukast is a leukotriene receptor antagonist that may be used in addition to ICSs for an additive effect.<br />
Can be of benefit in exercise-induced asthma and in people who also have rhinitis. Special Authority needed.<br />
Ipratropium reduces mucous secretions and relaxes airway muscle. It is short-acting and has a slower onset of<br />
action than beta2-agonists so is used more in COPD, although certain asthma patients may benefit. Longer<br />
acting antimuscarinic bronchodilators include tiotropium, glycopyrronium, umeclidinium, and aclidinium.<br />
Long-acting bronchodilators. Do not treat the underlying inflammation but may be beneficial in mild to<br />
moderate asthma instead of using higher doses of ICS. Used in conjunction with an ICS. Not useful for acute<br />
asthma attacks since they do not open airways immediately. Do not exceed recommended dose.<br />
Combination agents may aid adherence to recommended preventative regimens.<br />
Please refer to detailed product information as well as asthma guidelines to distinguish when combination<br />
inhalers should be used, and which combinations are recommended depending on the severity of the asthma<br />
or COPD.<br />
Dispense<br />
Ventolin ®<br />
The original blue inhaler<br />
that Kiwis know and trust 2<br />
Help to improve delivery of MDIs to the lungs, reduce adverse effects of ICSs. Wash once a week with warm<br />
water and a squirt of detergent and allow to completely drip dry. This leaves a slight residue of detergent<br />
on the inside of the spacer which reduces static and stops the medicine in the inhaler sticking to the sides.<br />
Replace every six to 12 months (tiny scratches or abrasions can prevent the spacer working as effectively).<br />
VENTOLIN<br />
Asthma<br />
Symptom Relief<br />
doesn’t need to involve an<br />
unpleasant aftertaste. 1<br />
DISPENSE<br />
ALCOHOL<br />
FREE<br />
VENTOLIN 2<br />
Page VEN_XXXX_Ventoline 16 HEALTHCARE Strip Ad Marc HANDBOOK 17 V3.indd 1 <strong>2017</strong>-2018 Common Disorders