Volume 11 Issue 1 (February) - Australasian Society for Ultrasound ...
Volume 11 Issue 1 (February) - Australasian Society for Ultrasound ...
Volume 11 Issue 1 (February) - Australasian Society for Ultrasound ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
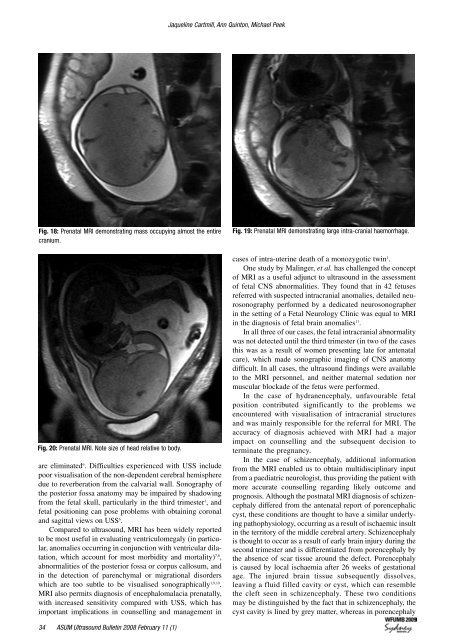
Jaqueline Cartmill, Ann Quinton, Michael Peek<br />
Fig. 18: Prenatal MRI demonstrating mass occupying almost the entire<br />
cranium.<br />
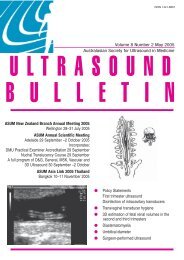
Fig. 20: Prenatal MRI. Note size of head relative to body.<br />
are eliminated 6 . Difficulties experienced with USS include<br />
poor visualisation of the non-dependent cerebral hemisphere<br />
due to reverberation from the calvarial wall. Sonography of<br />
the posterior fossa anatomy may be impaired by shadowing<br />
from the fetal skull, particularly in the third trimester 1 , and<br />
fetal positioning can pose problems with obtaining coronal<br />
and sagittal views on USS 6 .<br />
Compared to ultrasound, MRI has been widely reported<br />
to be most useful in evaluating ventriculomegaly (in particular,<br />
anomalies occurring in conjunction with ventricular dilatation,<br />
which account <strong>for</strong> most morbidity and mortality) 7,8 ,<br />
abnormalities of the posterior fossa or corpus callosum, and<br />
in the detection of parenchymal or migrational disorders<br />
which are too subtle to be visualised sonographically 1,9,10 .<br />
MRI also permits diagnosis of encephalomalacia prenatally,<br />
with increased sensitivity compared with USS, which has<br />
important implications in counselling and management in<br />
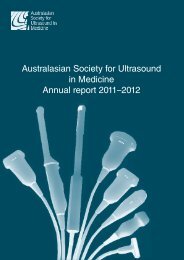
Fig. 19: Prenatal MRI demonstrating large intra-cranial haemorrhage.<br />
cases of intra-uterine death of a monozygotic twin 1 .<br />
One study by Malinger, et al. has challenged the concept<br />
of MRI as a useful adjunct to ultrasound in the assessment<br />
of fetal CNS abnormalities. They found that in 42 fetuses<br />
referred with suspected intracranial anomalies, detailed neurosonography<br />
per<strong>for</strong>med by a dedicated neurosonographer<br />
in the setting of a Fetal Neurology Clinic was equal to MRI<br />
in the diagnosis of fetal brain anomalies <strong>11</strong> .<br />
In all three of our cases, the fetal intracranial abnormality<br />
was not detected until the third trimester (in two of the cases<br />
this was as a result of women presenting late <strong>for</strong> antenatal<br />
care), which made sonographic imaging of CNS anatomy<br />
difficult. In all cases, the ultrasound findings were available<br />
to the MRI personnel, and neither maternal sedation nor<br />
muscular blockade of the fetus were per<strong>for</strong>med.<br />
In the case of hydranencephaly, unfavourable fetal<br />
position contributed significantly to the problems we<br />
encountered with visualisation of intracranial structures<br />
and was mainly responsible <strong>for</strong> the referral <strong>for</strong> MRI. The<br />
accuracy of diagnosis achieved with MRI had a major<br />
impact on counselling and the subsequent decision to<br />
terminate the pregnancy.<br />
In the case of schizencephaly, additional in<strong>for</strong>mation<br />
from the MRI enabled us to obtain multidisciplinary input<br />
from a paediatric neurologist, thus providing the patient with<br />
more accurate counselling regarding likely outcome and<br />
prognosis. Although the postnatal MRI diagnosis of schizencephaly<br />
differed from the antenatal report of porencephalic<br />
cyst, these conditions are thought to have a similar underlying<br />
pathophysiology, occurring as a result of ischaemic insult<br />
in the territory of the middle cerebral artery. Schizencephaly<br />
is thought to occur as a result of early brain injury during the<br />
second trimester and is differentiated from porencephaly by<br />
the absence of scar tissue around the defect. Porencephaly<br />
is caused by local ischaemia after 26 weeks of gestational<br />
age. The injured brain tissue subsequently dissolves,<br />
leaving a fluid filled cavity or cyst, which can resemble<br />
the cleft seen in schizencephaly. These two conditions<br />
may be distinguished by the fact that in schizencephaly, the<br />
cyst cavity is lined by grey matter, whereas in porencephaly<br />
4 ASUM <strong>Ultrasound</strong> Bulletin 2008 <strong>February</strong> <strong>11</strong> (1)