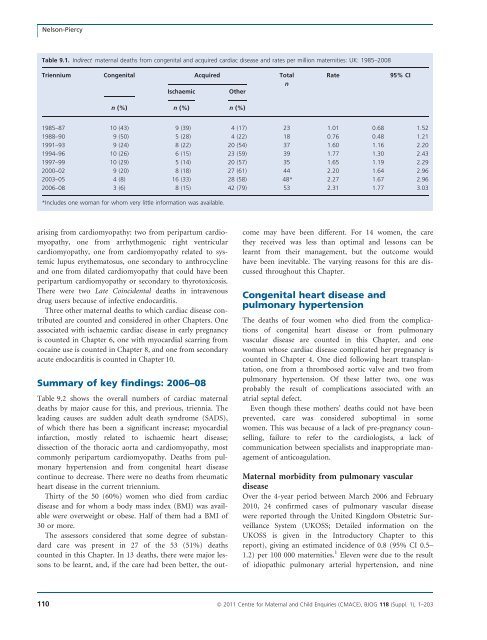
Nelson-PiercyTable 9.1. Indirect <strong>maternal</strong> <strong>deaths</strong> from congenital and acquired cardiac disease and rates per million maternities: UK: 1985–<strong>2008</strong>Triennium Congenital Acquired TotalnIschaemicOtherRate95% CIn (%) n (%) n (%)1985–87 10 (43) 9 (39) 4 (17) 23 1.01 0.68 1.521988–90 9 (50) 5 (28) 4 (22) 18 0.76 0.48 1.211991–93 9 (24) 8 (22) 20 (54) 37 1.60 1.16 2.201994–96 10 (26) 6 (15) 23 (59) 39 1.77 1.30 2.431997–99 10 (29) 5 (14) 20 (57) 35 1.65 1.19 2.292000–02 9 (20) 8 (18) 27 (61) 44 2.20 1.64 2.962003–05 4 (8) 16 (33) 28 (58) 48* 2.27 1.67 2.96<strong>2006</strong>–08 3 (6) 8 (15) 42 (79) 53 2.31 1.77 3.03*Includes one woman for whom very little information was available.arising from cardiomyopathy: two from peripartum cardiomyopathy,one from arrhythmogenic right ventricularcardiomyopathy, one from cardiomyopathy related <strong>to</strong> systemiclupus erythema<strong>to</strong>sus, one secondary <strong>to</strong> anthrocyclineand one from dilated cardiomyopathy that could have beenperipartum cardiomyopathy or secondary <strong>to</strong> thyro<strong>to</strong>xicosis.There were two Late Coincidental <strong>deaths</strong> in intravenousdrug users because of infective endocarditis.Three other <strong>maternal</strong> <strong>deaths</strong> <strong>to</strong> which cardiac disease contributedare counted and considered in other Chapters. Oneassociated with ischaemic cardiac disease in early pregnancyis counted in Chapter 6, one with myocardial scarring fromcocaine use is counted in Chapter 8, and one from secondaryacute endocarditis is counted in Chapter 10.Summary of key findings: <strong>2006</strong>–08Table 9.2 shows the overall numbers of cardiac <strong>maternal</strong><strong>deaths</strong> by major cause for this, and previous, triennia. Theleading causes are sudden adult death syndrome (SADS),of which there has been a significant increase; myocardialinfarction, mostly related <strong>to</strong> ischaemic heart disease;dissection of the thoracic aorta and cardiomyopathy, mostcommonly peripartum cardiomyopathy. Deaths from pulmonaryhypertension and from congenital heart diseasecontinue <strong>to</strong> decrease. There were no <strong>deaths</strong> from rheumaticheart disease in the current triennium.Thirty of the 50 (60%) women who died from cardiacdisease and for whom a body mass index (BMI) was availablewere overweight or obese. Half of them had a BMI of30 or more.The assessors considered that some degree of substandardcare was present in 27 of the 53 (51%) <strong>deaths</strong>counted in this Chapter. In 13 <strong>deaths</strong>, there were major lessons<strong>to</strong> be learnt, and, if the care had been better, the outcomemay have been different. For 14 women, the carethey received was less than optimal and lessons can belearnt from their management, but the outcome wouldhave been inevitable. The varying reasons for this are discussedthroughout this Chapter.Congenital heart disease andpulmonary hypertensionThe <strong>deaths</strong> of four women who died from the complicationsof congenital heart disease or from pulmonaryvascular disease are counted in this Chapter, and onewoman whose cardiac disease complicated her pregnancy iscounted in Chapter 4. One died following heart transplantation,one from a thrombosed aortic valve and two frompulmonary hypertension. Of these latter two, one wasprobably the result of complications associated with anatrial septal defect.Even though these mothers’ <strong>deaths</strong> could not have beenprevented, care was considered suboptimal in somewomen. This was because of a lack of pre-pregnancy counselling,failure <strong>to</strong> refer <strong>to</strong> the cardiologists, a lack ofcommunication between specialists and inappropriate managemen<strong>to</strong>f anticoagulation.Maternal morbidity from pulmonary vasculardiseaseOver the 4-year period between <strong>March</strong> <strong>2006</strong> and February2010, 24 confirmed cases of pulmonary vascular diseasewere reported through the United Kingdom Obstetric SurveillanceSystem (UKOSS; Detailed information on theUKOSS is given in the Introduc<strong>to</strong>ry Chapter <strong>to</strong> thisreport), giving an estimated incidence of 0.8 (95% CI 0.5–1.2) per 100 000 maternities. 1 Eleven were due <strong>to</strong> the resul<strong>to</strong>f idiopathic pulmonary arterial hypertension, and nine110 ª <strong>2011</strong> Centre for Maternal and Child Enquiries (CMACE), BJOG 118 (Suppl. 1), 1–203
Chapter 9: Cardiac diseaseTable 9.2. Causes of <strong>maternal</strong> death from cardiac disease; UK: 1994–<strong>2008</strong>Type and cause of death 1994–96 1997–99 2000–02 2003–05 <strong>2006</strong>–08AcquiredAortic dissection 7 5 7 9 7Myocardial infarction (MI) 6 5 8 12 6Ischaemic heart disease (no MI) 0 0 0 4 5Sudden adult death syndrome (SADS) 0 0 4 3 10Peripartum cardiomyopathy 4 7 4 0* 9**Other cardiomyopathy 2 3 4 1 4Myocarditis or myocardial fibrosis 3 2 3 5 4Mitral stenosis or valve disease 0 0 3 3 0Thrombosed aortic or tricuspid valve 1 0 0 0 2Infective endocarditis 0 2 1 2 2Right or left ventricular hypertrophy or1 2 2 2 1hypertensive heart diseaseCongenitalPulmonary hypertension (PHT) 7 7 4 3 2Congenital heart disease (not PHT or3 2 2 3 1thrombosed aortic valve)Other 5 0 2 0 0Total 39 35 44 48*** 53*Twelve Late <strong>deaths</strong> reported in 2003–05.**Two Late <strong>deaths</strong> reported in <strong>2006</strong>–08.***Includes one woman for whom information on cause was not available.were attributed <strong>to</strong> congenital heart disease. There were tworelated <strong>to</strong> chronic thromboembolism, one <strong>to</strong> sleep apnoeaand one <strong>to</strong> connective tissue disease. Fourteen cases wereknown before pregnancy and ten were diagnosed duringpregnancy.Acquired heart diseaseMyocardial infarction and ischaemic heart diseaseEleven women died from acute myocardial infarction (MI)or chronic ischaemic heart disease (IHD), a rate of 0.48(95% CI 0.27–0.87) per 100 000 maternities compared withthe 16 whose <strong>deaths</strong> were considered in the last Report, arate of 0.76 (95% CI 0.46–1.2) per 100 000 maternities.Coronary atheroma was the underlying pathology in threeof the six women who died from MI; one of these <strong>deaths</strong>was the result of extensive coronary artery dissection, arecognised complication of pregnancy and in the two otherwomen the cause of death was undetermined. There werealso five <strong>deaths</strong> from IHD where no acute MI was demonstrated.Presumably death in these women related <strong>to</strong>arrhythmia or heart failure. In <strong>to</strong>tal, eight women died fromIHD compared with 12 in the previous triennium.The women who diedAgain, as shown in the last Report, the impact of lifestylefac<strong>to</strong>rs such as increasing <strong>maternal</strong> age, obesity and smokingwas dramatic, and all of the women who died had identifiablerisk fac<strong>to</strong>rs. The mothers’ ages ranged from 28 <strong>to</strong>46 years with a median of 36 years. Eight women were 35or older, of whom five were aged 40 years or more. All wereparous, and seven were para 4 or greater, of whom twowere of extremely high parity. Six smoked, four had knownhypertension, four were overweight and three were obese.Two had a family his<strong>to</strong>ry of cardiac disease, one had hypercholesterolaemia,one had gestational diabetes and one hadsickle cell disease. Three women were from black andminority ethnic groups. Three mothers also had social problems:two were known <strong>to</strong> the child protection services, oneof whom had also reported domestic violence, and anotherwoman abused cannabis and alcohol.All but two of these women died postnatally, althoughone had collapsed antenatally near term.Maternal morbidity from acute myocardialinfarctionThe UKOSS study of acute MI in pregnancy, undertakenbetween August 2005 and February 2010, 1 identified 23confirmed nonfatal cases occurring antenatally, giving anestimated incidence of 0.7 (95% CI 0.4–1.0) cases per100 000 maternities. Fourteen of the women with a confirmedMI had angiography: seven had coronary atheroma,three had coronary artery dissection, two hadcoronary arterial thrombosis and two had normal coro-ª <strong>2011</strong> Centre for Maternal and Child Enquiries (CMACE), BJOG 118 (Suppl. 1), 1–203 111
- Page 1:
Volume 118, Supplement 1, March 201
- Page 4 and 5:
AcknowledgementsSaving Mothers’ L
- Page 6 and 7:
AcknowledgementsAcknowledgementsCMA
- Page 8 and 9:
Forewordbeen written jointly by a m
- Page 10 and 11:
‘Top ten’ recommendationsServic
- Page 12 and 13:
‘Top ten’ recommendationscommun
- Page 14 and 15:
‘Top ten’ recommendationsof suc
- Page 16 and 17:
‘Top ten’ recommendationsMarch
- Page 18 and 19:
Oates et al.Back to basicsM Oates 1
- Page 20 and 21:
Oates et al.BreathlessnessBreathles
- Page 22 and 23:
Oates et al.appropriate pathway of
- Page 24 and 25:
LewisIntroduction: Aims, objectives
- Page 26 and 27:
LewisAn important limitation of ran
- Page 28 and 29:
Lewismaternal and public health-pol
- Page 30 and 31:
Lewisresult in a live birth at any
- Page 32 and 33:
LewisChapter 1: The women who died
- Page 34 and 35:
Lewiswho would not have been identi
- Page 36 and 37:
Lewis1098Rate per 100 000 materniti
- Page 38 and 39:
LewisTable 1.4. Numbers and rates o
- Page 40 and 41:
Lewis2.50Rate per 100 000 materniti
- Page 42 and 43:
LewisTable 1.9. Number of maternal
- Page 44 and 45:
LewisTable 1.12. Numbers and percen
- Page 46 and 47:
LewisThere were cases where a major
- Page 48 and 49:
LewisBox 1.5. Classifications of Bo
- Page 50 and 51:
LewisTable 1.20. Number and estimat
- Page 52 and 53:
LewisNew countries of the European
- Page 54 and 55:
LewisTable 1.23. Direct and Indirec
- Page 56 and 57:
LewisTable 1.26. Characteristics* o
- Page 58 and 59:
Lewis4 Lewis G (ed). The Confidenti
- Page 60 and 61:
DrifeTable 2.1. Direct deaths from
- Page 62 and 63: Drifewomen who died in 2006-08 had
- Page 64 and 65: Drifedelivery she became breathless
- Page 66 and 67: DrifePathological overviewFourteen
- Page 68 and 69: NeilsonChapter 3: Pre-eclampsia and
- Page 70 and 71: Neilsontrue, and what might be the
- Page 72 and 73: NeilsonConclusionThe number of deat
- Page 74 and 75: NormanBackgroundIn the UK, major ob
- Page 76 and 77: Normanwhich there was catastrophic
- Page 78 and 79: Normanrecommendations made in succe
- Page 80 and 81: DawsonBox 5.1. The UK amniotic flui
- Page 82 and 83: Dawsontry despite an extensive sear
- Page 84 and 85: O’HerlihyTable 6.1. Numbers of Di
- Page 86 and 87: O’Herlihytoxic shock syndrome aft
- Page 88 and 89: HarperGroup A b-haemolytic streptoc
- Page 90 and 91: Harperthe 6-week postnatal period,
- Page 92 and 93: Harpera major intrapartum haemorrha
- Page 94 and 95: HarperBox 7.1. Signs and symptoms o
- Page 96 and 97: Harperwoman was given several litre
- Page 98 and 99: Harper2 Lamagni TL, Efstratiou A, D
- Page 100 and 101: LucasTable A7.1 Proposed new catego
- Page 102 and 103: Lucasthe same infection scenario as
- Page 104 and 105: McClure, CooperChapter 8: Anaesthes
- Page 106 and 107: McClure, Cooperaddress, but protoco
- Page 108 and 109: McClure, CooperPostpartum haemorrha
- Page 110 and 111: McClure, CooperWorkloadA number of
- Page 114 and 115: Nelson-Piercynary arteries. In view
- Page 116 and 117: Nelson-Piercynormal left ventricle
- Page 118 and 119: LucasAnnex 9.1. Pathological overvi
- Page 120 and 121: Lucasdiac death that is non-ischaem
- Page 122 and 123: de Swiet et al.causes but are aggra
- Page 124 and 125: de Swiet et al.died of SUDEP before
- Page 126 and 127: de Swiet et al.for 6 weeks after de
- Page 128 and 129: de Swiet et al.mised. The obstetric
- Page 130 and 131: de Swiet et al.CancerPregnancy does
- Page 132 and 133: de Swiet et al.a thorough autopsy w
- Page 134 and 135: Oates, CantwellChapter 11: Deaths f
- Page 136 and 137: Oates, CantwellTable 11.1. Timing o
- Page 138 and 139: Oates, CantwellTable 11.5. Maternal
- Page 140 and 141: Oates, CantwellChild protection iss
- Page 142 and 143: Oates, CantwellAll women who are su
- Page 144 and 145: Oates, Cantwell4 Kendel RE, Chalmer
- Page 146 and 147: Lewismaternal mortality rates or ra
- Page 148 and 149: Annex 12.1. Domestic abuseAnnex 12.
- Page 150 and 151: Annex 12.1. Domestic abuseshe could
- Page 152 and 153: Garrod et al.supportive but challen
- Page 154 and 155: Garrod et al.• Culture and system
- Page 156 and 157: Garrod et al.the second stage and s
- Page 158 and 159: Garrod et al.through the still heal
- Page 160 and 161: ShakespeareChapter 14: General prac
- Page 162 and 163:
Shakespeareemergency caesarean sect
- Page 164 and 165:
ShakespeareCardiac diseaseDeaths fr
- Page 166 and 167:
Shakespearereduce the risks to the
- Page 168 and 169:
ShakespeareManaging a maternal deat
- Page 170 and 171:
Hulbertin the ED was of a high qual
- Page 172 and 173:
HulbertPre-eclampsia/eclampsia: lea
- Page 174 and 175:
HulbertTransfersWhen the obstetric
- Page 176 and 177:
Clutton-Brocksimply the case that s
- Page 178 and 179:
Clutton-BrockDiagnosis of sepsisTak
- Page 180 and 181:
Clutton-Brockpulseless electrical a
- Page 182 and 183:
Clutton-BrockImprovement Scotland (
- Page 184 and 185:
Lucas, Millward-Sadler95 mmHg. This
- Page 186 and 187:
Lucas, Millward-Sadleran agreed mai
- Page 188 and 189:
Annex 17.1. The main clinico-tholog
- Page 190 and 191:
MillerAppendix 1: The method of Enq
- Page 192 and 193:
MillerDatanotificationNotificationR
- Page 194 and 195:
Knight• investigating different m
- Page 196 and 197:
Knightbaseline incidence against wh
- Page 198 and 199:
LennoxAppendix 2B: Summary of Scott
- Page 200 and 201:
LennoxEvidence of effective managem
- Page 202 and 203:
Appendix 3: Contributors to the Mat
- Page 204 and 205:
Appendix 3: Contributors to the Mat