6.-March-2011-Saving-Mothers-Lives-reviewing-maternal-deaths-to-make-motherhood-safer-2006-2008
6.-March-2011-Saving-Mothers-Lives-reviewing-maternal-deaths-to-make-motherhood-safer-2006-2008
6.-March-2011-Saving-Mothers-Lives-reviewing-maternal-deaths-to-make-motherhood-safer-2006-2008
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
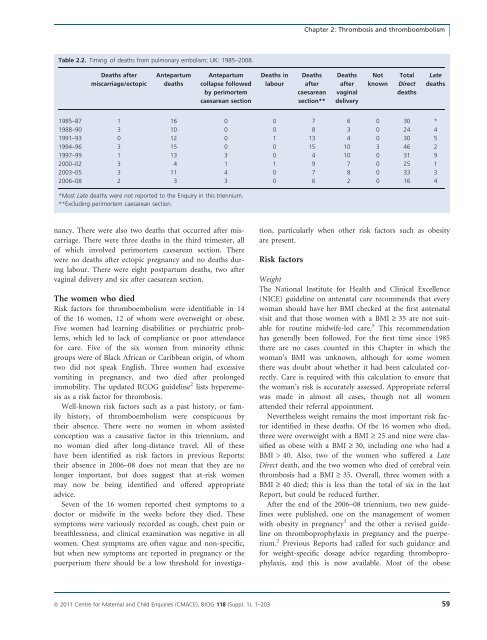
Chapter 2: Thrombosis and thromboembolismTable 2.2. Timing of <strong>deaths</strong> from pulmonary embolism; UK: 1985–<strong>2008</strong>.Deaths aftermiscarriage/ec<strong>to</strong>picAntepartum<strong>deaths</strong>Antepartumcollapse followedby perimortemcaesarean sectionDeaths inlabourDeathsaftercaesareansection**DeathsaftervaginaldeliveryNotknownTotalDirect<strong>deaths</strong>Late<strong>deaths</strong>1985–87 1 16 0 0 7 6 0 30 *1988–90 3 10 0 0 8 3 0 24 41991–93 0 12 0 1 13 4 0 30 51994–96 3 15 0 0 15 10 3 46 21997–99 1 13 3 0 4 10 0 31 92000–02 3 4 1 1 9 7 0 25 12003–05 3 11 4 0 7 8 0 33 3<strong>2006</strong>–08 2 3 3 0 6 2 0 16 4*Most Late <strong>deaths</strong> were not reported <strong>to</strong> the Enquiry in this triennium.**Excluding perimortem caesarean section.nancy. There were also two <strong>deaths</strong> that occurred after miscarriage.There were three <strong>deaths</strong> in the third trimester, allof which involved perimortem caesarean section. Therewere no <strong>deaths</strong> after ec<strong>to</strong>pic pregnancy and no <strong>deaths</strong> duringlabour. There were eight postpartum <strong>deaths</strong>, two aftervaginal delivery and six after caesarean section.The women who diedRisk fac<strong>to</strong>rs for thromboembolism were identifiable in 14of the 16 women, 12 of whom were overweight or obese.Five women had learning disabilities or psychiatric problems,which led <strong>to</strong> lack of compliance or poor attendancefor care. Five of the six women from minority ethnicgroups were of Black African or Caribbean origin, of whomtwo did not speak English. Three women had excessivevomiting in pregnancy, and two died after prolongedimmobility. The updated RCOG guideline 2 lists hyperemesisas a risk fac<strong>to</strong>r for thrombosis.Well-known risk fac<strong>to</strong>rs such as a past his<strong>to</strong>ry, or familyhis<strong>to</strong>ry, of thromboembolism were conspicuous bytheir absence. There were no women in whom assistedconception was a causative fac<strong>to</strong>r in this triennium, andno woman died after long-distance travel. All of thesehave been identified as risk fac<strong>to</strong>rs in previous Reports:their absence in <strong>2006</strong>–08 does not mean that they are nolonger important, but does suggest that at-risk womenmay now be being identified and offered appropriateadvice.Seven of the 16 women reported chest symp<strong>to</strong>ms <strong>to</strong> adoc<strong>to</strong>r or midwife in the weeks before they died. Thesesymp<strong>to</strong>ms were variously recorded as cough, chest pain orbreathlessness, and clinical examination was negative in allwomen. Chest symp<strong>to</strong>ms are often vague and non-specific,but when new symp<strong>to</strong>ms are reported in pregnancy or thepuerperium there should be a low threshold for investigation,particularly when other risk fac<strong>to</strong>rs such as obesityare present.Risk fac<strong>to</strong>rsWeightThe National Institute for Health and Clinical Excellence(NICE) guideline on antenatal care recommends that everywoman should have her BMI checked at the first antenatalvisit and that those women with a BMI ‡ 35 are not suitablefor routine midwife-led care. 5 This recommendationhas generally been followed. For the first time since 1985there are no cases counted in this Chapter in which thewoman’s BMI was unknown, although for some womenthere was doubt about whether it had been calculated correctly.Care is required with this calculation <strong>to</strong> ensure thatthe woman’s risk is accurately assessed. Appropriate referralwas made in almost all cases, though not all womenattended their referral appointment.Nevertheless weight remains the most important risk fac<strong>to</strong>ridentified in these <strong>deaths</strong>. Of the 16 women who died,three were overweight with a BMI ‡ 25 and nine were classifiedas obese with a BMI ‡ 30, including one who had aBMI > 40. Also, two of the women who suffered a LateDirect death, and the two women who died of cerebral veinthrombosis had a BMI ‡ 35. Overall, three women with aBMI ‡ 40 died; this is less than the <strong>to</strong>tal of six in the lastReport, but could be reduced further.After the end of the <strong>2006</strong>–08 triennium, two new guidelineswere published, one on the management of womenwith obesity in pregnancy 1 and the other a revised guidelineon thromboprophylaxis in pregnancy and the puerperium.2 Previous Reports had called for such guidance andfor weight-specific dosage advice regarding thromboprophylaxis,and this is now available. Most of the obeseª <strong>2011</strong> Centre for Maternal and Child Enquiries (CMACE), BJOG 118 (Suppl. 1), 1–203 59