Dawsontry despite an extensive search. This case was acceptedbecause the quality of the au<strong>to</strong>psy report suggested tha<strong>to</strong>ther possible causes had been reasonably excluded. If true,it suggests that squames are a common surrogate markerfor the syndrome but not necessarily its precipitating cause.ConclusionsAmniotic fluid embolism, particularly if the collapse happensin a well-equipped unit, should now be considered a treatableand survivable event in the majority of cases. It has nowfallen <strong>to</strong> fourth place among causes of Direct <strong>maternal</strong> <strong>deaths</strong>but nevertheless continues <strong>to</strong> be a significant fac<strong>to</strong>r in <strong>maternal</strong>mortality rates in the UK. The clinical presentation ofAFE can be confused with other causes of collapse, but effectiveresuscitation remains the essential common responseirrespective of the underlying cause for collapse.When a death does occur, a detailed prompt au<strong>to</strong>psyshould be performed that includes immunochemistry orhis<strong>to</strong>chemistry. All cases, fatal or not, should be reported<strong>to</strong> UKOSS.Disclosure of interestsNone.FundingThis work was undertaken by the Centre for Maternal andChild Enquiries (CMACE) as part of the CEMACH programme.The work was funded by the National PatientSafety Agency; the Department of Health, Social Servicesand Public Safety of Northern Ireland; NHS QualityImprovement Scotland (NHS QIS); and the ChannelIslands and Isle of Man.AcknowledgementsThis Chapter had been seen and discussed with Mr DerelTuffnell, Consultant in Obstetrics and Gynaecology ofBradford Royal Infirmary and Dr Marian Knight, Head ofUKOSS and Senior Clinical Research Fellow for the NPEU.The Pathology overview was written by Dr H Hillward-Sadler, Consultant His<strong>to</strong>pathologist of Southamp<strong>to</strong>n UniversityHospitals NHS Trust. jReferences1 Knight M, Tuffnell D, Brocklehurst P, Spark P, Kurinczuk JJ. Incidenceand risk fac<strong>to</strong>rs for amniotic-fluid embolism. Obstet Gynecol2010;115:910–7.2 Department of Health Report on Confidential Enquiries in<strong>to</strong> MaternalDeaths in the United Kingdom 1991–1993. London: HMSO, 1995.3 Lewis G, edi<strong>to</strong>r; The Confidential Enquiry in<strong>to</strong> Maternal and ChildHealth (CEMACH). <strong>Saving</strong> <strong>Mothers</strong>’ <strong>Lives</strong>: Reviewing Maternal Deaths<strong>to</strong> Make Motherhood Safer—2003–2005. The Seventh Report onConfidential Enquiries in<strong>to</strong> Maternal Deaths in the United Kingdom.London: CEMACH, 2007. [www.cmace.org.uk]. Accessed 5 Oc<strong>to</strong>ber2010.4 English Births. [www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=1022]. Accessed 7 April 2010.5 Scottish Births. [www.isdscotland.org/isd/1612.html]. Accessed 7 April2010.6 Welsh births. [wales.gov.uk/<strong>to</strong>pics/statistics/headlines/health2010/0210/?lang=en] Accessed 7 April 2010.7 Howell C, Grady K, Cox C, edi<strong>to</strong>rs. Managing Obstetric Emergenciesand Trauma—the MOET Course Manual, 2nd edn. London: RCOG,2007.80 ª <strong>2011</strong> Centre for Maternal and Child Enquiries (CMACE), BJOG 118 (Suppl. 1), 1–203
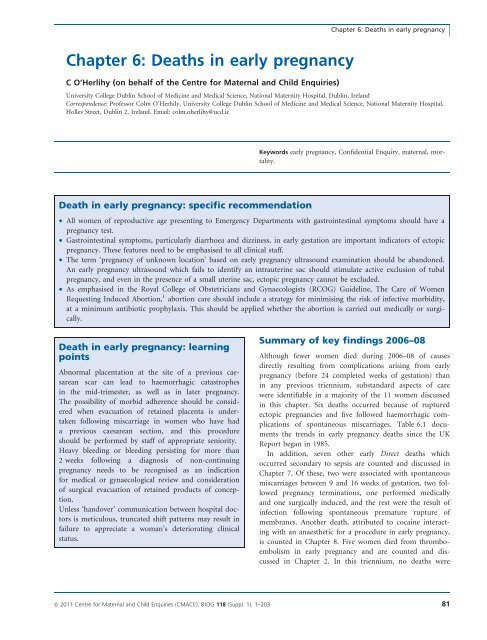
Chapter 6: Deaths in early pregnancyChapter 6: Deaths in early pregnancyC O’Herlihy (on behalf of the Centre for Maternal and Child Enquiries)University College Dublin School of Medicine and Medical Science, National Maternity Hospital, Dublin, IrelandCorrespondence: Professor Colm O’Herhily, University College Dublin School of Medicine and Medical Science, National Maternity Hospital,Holles Street, Dublin 2, Ireland. Email: colm.oherlihy@ucd.ieKeywords early pregnancy, Confidential Enquiry, <strong>maternal</strong>, mortality.Death in early pregnancy: specific recommendation• All women of reproductive age presenting <strong>to</strong> Emergency Departments with gastrointestinal symp<strong>to</strong>ms should have apregnancy test.• Gastrointestinal symp<strong>to</strong>ms, particularly diarrhoea and dizziness, in early gestation are important indica<strong>to</strong>rs of ec<strong>to</strong>picpregnancy. These features need <strong>to</strong> be emphasised <strong>to</strong> all clinical staff.• The term ‘pregnancy of unknown location’ based on early pregnancy ultrasound examination should be abandoned.An early pregnancy ultrasound which fails <strong>to</strong> identify an intrauterine sac should stimulate active exclusion of tubalpregnancy, and even in the presence of a small uterine sac, ec<strong>to</strong>pic pregnancy cannot be excluded.• As emphasised in the Royal College of Obstetricians and Gynaecologists (RCOG) Guideline, The Care of WomenRequesting Induced Abortion, 1 abortion care should include a strategy for minimising the risk of infective morbidity,at a minimum antibiotic prophylaxis. This should be applied whether the abortion is carried out medically or surgically.Death in early pregnancy: learningpointsAbnormal placentation at the site of a previous caesareanscar can lead <strong>to</strong> haemorrhagic catastrophesin the mid-trimester, as well as in later pregnancy.The possibility of morbid adherence should be consideredwhen evacuation of retained placenta is undertakenfollowing miscarriage in women who have hada previous caesarean section, and this procedureshould be performed by staff of appropriate seniority.Heavy bleeding or bleeding persisting for more than2 weeks following a diagnosis of non-continuingpregnancy needs <strong>to</strong> be recognised as an indicationfor medical or gynaecological review and considerationof surgical evacuation of retained products of conception.Unless ‘handover’ communication between hospital doc<strong>to</strong>rsis meticulous, truncated shift patterns may result infailure <strong>to</strong> appreciate a woman’s deteriorating clinicalstatus.Summary of key findings <strong>2006</strong>–08Although fewer women died during <strong>2006</strong>–08 of causesdirectly resulting from complications arising from earlypregnancy (before 24 completed weeks of gestation) thanin any previous triennium, substandard aspects of carewere identifiable in a majority of the 11 women discussedin this chapter. Six <strong>deaths</strong> occurred because of rupturedec<strong>to</strong>pic pregnancies and five followed haemorrhagic complicationsof spontaneous miscarriages. Table <strong>6.</strong>1 documentsthe trends in early pregnancy <strong>deaths</strong> since the UKReport began in 1985.In addition, seven other early Direct <strong>deaths</strong> whichoccurred secondary <strong>to</strong> sepsis are counted and discussed inChapter 7. Of these, two were associated with spontaneousmiscarriages between 9 and 16 weeks of gestation, two followedpregnancy terminations, one performed medicallyand one surgically induced, and the rest were the result ofinfection following spontaneous premature rupture ofmembranes. Another death, attributed <strong>to</strong> cocaine interactingwith an anaesthetic for a procedure in early pregnancy,is counted in Chapter 8. Five women died from thromboembolismin early pregnancy and are counted and discussedin Chapter 2. In this triennium, no <strong>deaths</strong> wereª <strong>2011</strong> Centre for Maternal and Child Enquiries (CMACE), BJOG 118 (Suppl. 1), 1–203 81
- Page 1:
Volume 118, Supplement 1, March 201
- Page 4 and 5:
AcknowledgementsSaving Mothers’ L
- Page 6 and 7:
AcknowledgementsAcknowledgementsCMA
- Page 8 and 9:
Forewordbeen written jointly by a m
- Page 10 and 11:
‘Top ten’ recommendationsServic
- Page 12 and 13:
‘Top ten’ recommendationscommun
- Page 14 and 15:
‘Top ten’ recommendationsof suc
- Page 16 and 17:
‘Top ten’ recommendationsMarch
- Page 18 and 19:
Oates et al.Back to basicsM Oates 1
- Page 20 and 21:
Oates et al.BreathlessnessBreathles
- Page 22 and 23:
Oates et al.appropriate pathway of
- Page 24 and 25:
LewisIntroduction: Aims, objectives
- Page 26 and 27:
LewisAn important limitation of ran
- Page 28 and 29:
Lewismaternal and public health-pol
- Page 30 and 31:
Lewisresult in a live birth at any
- Page 32 and 33: LewisChapter 1: The women who died
- Page 34 and 35: Lewiswho would not have been identi
- Page 36 and 37: Lewis1098Rate per 100 000 materniti
- Page 38 and 39: LewisTable 1.4. Numbers and rates o
- Page 40 and 41: Lewis2.50Rate per 100 000 materniti
- Page 42 and 43: LewisTable 1.9. Number of maternal
- Page 44 and 45: LewisTable 1.12. Numbers and percen
- Page 46 and 47: LewisThere were cases where a major
- Page 48 and 49: LewisBox 1.5. Classifications of Bo
- Page 50 and 51: LewisTable 1.20. Number and estimat
- Page 52 and 53: LewisNew countries of the European
- Page 54 and 55: LewisTable 1.23. Direct and Indirec
- Page 56 and 57: LewisTable 1.26. Characteristics* o
- Page 58 and 59: Lewis4 Lewis G (ed). The Confidenti
- Page 60 and 61: DrifeTable 2.1. Direct deaths from
- Page 62 and 63: Drifewomen who died in 2006-08 had
- Page 64 and 65: Drifedelivery she became breathless
- Page 66 and 67: DrifePathological overviewFourteen
- Page 68 and 69: NeilsonChapter 3: Pre-eclampsia and
- Page 70 and 71: Neilsontrue, and what might be the
- Page 72 and 73: NeilsonConclusionThe number of deat
- Page 74 and 75: NormanBackgroundIn the UK, major ob
- Page 76 and 77: Normanwhich there was catastrophic
- Page 78 and 79: Normanrecommendations made in succe
- Page 80 and 81: DawsonBox 5.1. The UK amniotic flui
- Page 84 and 85: O’HerlihyTable 6.1. Numbers of Di
- Page 86 and 87: O’Herlihytoxic shock syndrome aft
- Page 88 and 89: HarperGroup A b-haemolytic streptoc
- Page 90 and 91: Harperthe 6-week postnatal period,
- Page 92 and 93: Harpera major intrapartum haemorrha
- Page 94 and 95: HarperBox 7.1. Signs and symptoms o
- Page 96 and 97: Harperwoman was given several litre
- Page 98 and 99: Harper2 Lamagni TL, Efstratiou A, D
- Page 100 and 101: LucasTable A7.1 Proposed new catego
- Page 102 and 103: Lucasthe same infection scenario as
- Page 104 and 105: McClure, CooperChapter 8: Anaesthes
- Page 106 and 107: McClure, Cooperaddress, but protoco
- Page 108 and 109: McClure, CooperPostpartum haemorrha
- Page 110 and 111: McClure, CooperWorkloadA number of
- Page 112 and 113: Nelson-PiercyTable 9.1. Indirect ma
- Page 114 and 115: Nelson-Piercynary arteries. In view
- Page 116 and 117: Nelson-Piercynormal left ventricle
- Page 118 and 119: LucasAnnex 9.1. Pathological overvi
- Page 120 and 121: Lucasdiac death that is non-ischaem
- Page 122 and 123: de Swiet et al.causes but are aggra
- Page 124 and 125: de Swiet et al.died of SUDEP before
- Page 126 and 127: de Swiet et al.for 6 weeks after de
- Page 128 and 129: de Swiet et al.mised. The obstetric
- Page 130 and 131: de Swiet et al.CancerPregnancy does
- Page 132 and 133:
de Swiet et al.a thorough autopsy w
- Page 134 and 135:
Oates, CantwellChapter 11: Deaths f
- Page 136 and 137:
Oates, CantwellTable 11.1. Timing o
- Page 138 and 139:
Oates, CantwellTable 11.5. Maternal
- Page 140 and 141:
Oates, CantwellChild protection iss
- Page 142 and 143:
Oates, CantwellAll women who are su
- Page 144 and 145:
Oates, Cantwell4 Kendel RE, Chalmer
- Page 146 and 147:
Lewismaternal mortality rates or ra
- Page 148 and 149:
Annex 12.1. Domestic abuseAnnex 12.
- Page 150 and 151:
Annex 12.1. Domestic abuseshe could
- Page 152 and 153:
Garrod et al.supportive but challen
- Page 154 and 155:
Garrod et al.• Culture and system
- Page 156 and 157:
Garrod et al.the second stage and s
- Page 158 and 159:
Garrod et al.through the still heal
- Page 160 and 161:
ShakespeareChapter 14: General prac
- Page 162 and 163:
Shakespeareemergency caesarean sect
- Page 164 and 165:
ShakespeareCardiac diseaseDeaths fr
- Page 166 and 167:
Shakespearereduce the risks to the
- Page 168 and 169:
ShakespeareManaging a maternal deat
- Page 170 and 171:
Hulbertin the ED was of a high qual
- Page 172 and 173:
HulbertPre-eclampsia/eclampsia: lea
- Page 174 and 175:
HulbertTransfersWhen the obstetric
- Page 176 and 177:
Clutton-Brocksimply the case that s
- Page 178 and 179:
Clutton-BrockDiagnosis of sepsisTak
- Page 180 and 181:
Clutton-Brockpulseless electrical a
- Page 182 and 183:
Clutton-BrockImprovement Scotland (
- Page 184 and 185:
Lucas, Millward-Sadler95 mmHg. This
- Page 186 and 187:
Lucas, Millward-Sadleran agreed mai
- Page 188 and 189:
Annex 17.1. The main clinico-tholog
- Page 190 and 191:
MillerAppendix 1: The method of Enq
- Page 192 and 193:
MillerDatanotificationNotificationR
- Page 194 and 195:
Knight• investigating different m
- Page 196 and 197:
Knightbaseline incidence against wh
- Page 198 and 199:
LennoxAppendix 2B: Summary of Scott
- Page 200 and 201:
LennoxEvidence of effective managem
- Page 202 and 203:
Appendix 3: Contributors to the Mat
- Page 204 and 205:
Appendix 3: Contributors to the Mat