A decade later - Fundação Luso-Americana
A decade later - Fundação Luso-Americana
A decade later - Fundação Luso-Americana
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
54<br />
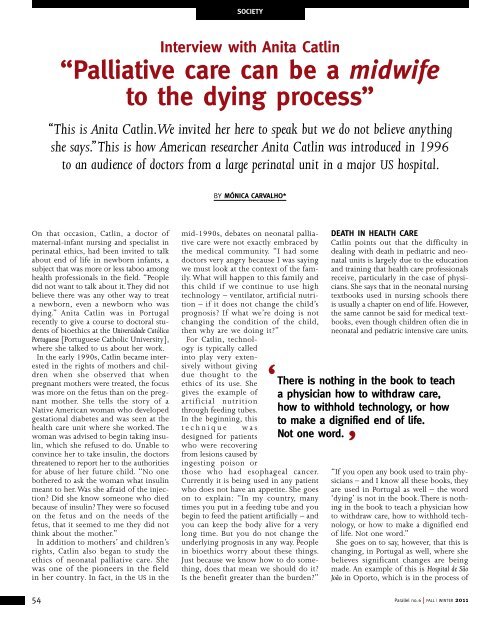
socieTy<br />
interview with Anita catlin<br />
“palliative care can be a midwife<br />
to the dying process”<br />
“This is Anita Catlin. We invited her here to speak but we do not believe anything<br />
she says.” This is how American researcher Anita Catlin was introduced in 1996<br />
to an audience of doctors from a large perinatal unit in a major US hospital.<br />
On that occasion, Catlin, a doctor of<br />
maternal-infant nursing and specialist in<br />
perinatal ethics, had been invited to talk<br />
about end of life in newborn infants, a<br />
subject that was more or less taboo among<br />
health professionals in the field. “People<br />
did not want to talk about it. They did not<br />
believe there was any other way to treat<br />
a newborn, even a newborn who was<br />
dying.” Anita Catlin was in Portugal<br />
recently to give a course to doctoral students<br />
of bioethics at the Universidade Católica<br />
Portuguesa [Portuguese Catholic University],<br />
where she talked to us about her work.<br />
In the early 1990s, Catlin became interested<br />
in the rights of mothers and children<br />
when she observed that when<br />
pregnant mothers were treated, the focus<br />
was more on the fetus than on the pregnant<br />
mother. She tells the story of a<br />
Native American woman who developed<br />
gestational diabetes and was seen at the<br />
health care unit where she worked. The<br />
woman was advised to begin taking insulin,<br />
which she refused to do. Unable to<br />
convince her to take insulin, the doctors<br />
threatened to report her to the authorities<br />
for abuse of her future child. “No one<br />
bothered to ask the woman what insulin<br />
meant to her. Was she afraid of the injection?<br />
Did she know someone who died<br />
because of insulin? They were so focused<br />
on the fetus and on the needs of the<br />
fetus, that it seemed to me they did not<br />
think about the mother.”<br />
In addition to mothers’ and children’s<br />
rights, Catlin also began to study the<br />
ethics of neonatal palliative care. She<br />
was one of the pioneers in the field<br />
in her country. In fact, in the US in the<br />
By mónicA cArvALHo*<br />
mid-1990s, debates on neonatal palliative<br />
care were not exactly embraced by<br />
the medical community. “I had some<br />
doctors very angry because I was saying<br />
we must look at the context of the family.<br />
What will happen to this family and<br />
this child if we continue to use high<br />
technology – ventilator, artificial nutrition<br />
– if it does not change the child’s<br />
prognosis? If what we’re doing is not<br />
changing the condition of the child,<br />
then why are we doing it?”<br />
For Catlin, technology<br />
is typically called<br />
into play very extensively<br />
without giving<br />
due thought to the<br />
ethics of its use. She<br />
gives the example of<br />
artificial nutrition<br />
through feeding tubes.<br />
In the beginning, this<br />
t e c h n i q u e w a s<br />
designed for patients<br />
who were recovering<br />
from lesions caused by<br />
ingesting poison or<br />
those who had esophageal cancer.<br />
Currently it is being used in any patient<br />
who does not have an appetite. She goes<br />
on to explain: “In my country, many<br />
times you put in a feeding tube and you<br />
begin to feed the patient artificially – and<br />
you can keep the body alive for a very<br />
long time. But you do not change the<br />
underlying prognosis in any way. People<br />
in bioethics worry about these things.<br />
Just because we know how to do something,<br />
does that mean we should do it?<br />
Is the benefit greater than the burden?”<br />
deATH in HeALTH cAre<br />
Catlin points out that the difficulty in<br />
dealing with death in pediatric and neonatal<br />
units is largely due to the education<br />
and training that health care professionals<br />
receive, particularly in the case of physicians.<br />
She says that in the neonatal nursing<br />
textbooks used in nursing schools there<br />
is usually a chapter on end of life. However,<br />
the same cannot be said for medical textbooks,<br />
even though children often die in<br />
neonatal and pediatric intensive care units.<br />
‘ There is nothing in the book to teach<br />
a physician how to withdraw care,<br />
how to withhold technology, or how<br />
to make a dignified end of life.<br />
not one word.<br />
’<br />
“If you open any book used to train physicians<br />
– and I know all these books, they<br />
are used in Portugal as well – the word<br />
‘dying’ is not in the book. There is nothing<br />
in the book to teach a physician how<br />
to withdraw care, how to withhold technology,<br />
or how to make a dignified end<br />
of life. Not one word.”<br />
She goes on to say, however, that this is<br />
changing, in Portugal as well, where she<br />
believes significant changes are being<br />
made. An example of this is Hospital de São<br />
João in Oporto, which is in the process of<br />
Parallel no. 6 | FALL | WINTER 2011