PART I - Department of Behavioral Health and Developmental ...
PART I - Department of Behavioral Health and Developmental ...
PART I - Department of Behavioral Health and Developmental ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
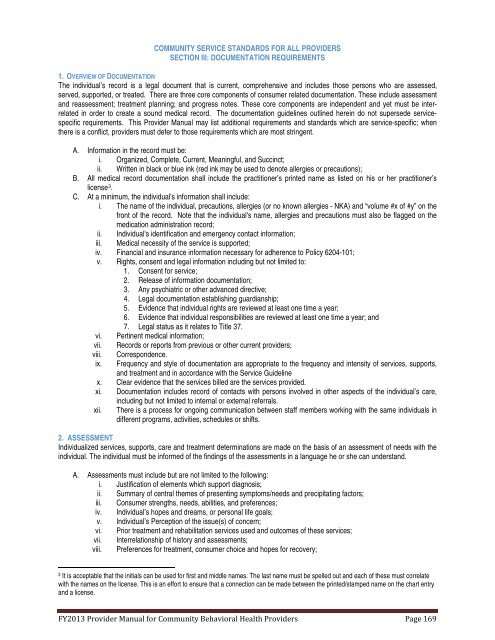
COMMUNITY SERVICE STANDARDS FOR ALL PROVIDERSSECTION III: DOCUMENTATION REQUIREMENTS1. OVERVIEW OF DOCUMENTATIONThe individual’s record is a legal document that is current, comprehensive <strong>and</strong> includes those persons who are assessed,served, supported, or treated. There are three core components <strong>of</strong> consumer related documentation. These include assessment<strong>and</strong> reassessment; treatment planning; <strong>and</strong> progress notes. These core components are independent <strong>and</strong> yet must be interrelatedin order to create a sound medical record. The documentation guidelines outlined herein do not supersede servicespecificrequirements. This Provider Manual may list additional requirements <strong>and</strong> st<strong>and</strong>ards which are service-specific; whenthere is a conflict, providers must defer to those requirements which are most stringent.A. Information in the record must be:i. Organized, Complete, Current, Meaningful, <strong>and</strong> Succinct;ii. Written in black or blue ink (red ink may be used to denote allergies or precautions);B. All medical record documentation shall include the practitioner’s printed name as listed on his or her practitioner’slicense 3 .C. At a minimum, the individual's information shall include:i. The name <strong>of</strong> the individual, precautions, allergies (or no known allergies - NKA) <strong>and</strong> “volume #x <strong>of</strong> #y” on thefront <strong>of</strong> the record. Note that the individual's name, allergies <strong>and</strong> precautions must also be flagged on themedication administration record;ii. Individual's identification <strong>and</strong> emergency contact information;iii. Medical necessity <strong>of</strong> the service is supported;iv. Financial <strong>and</strong> insurance information necessary for adherence to Policy 6204-101;v. Rights, consent <strong>and</strong> legal information including but not limited to:1. Consent for service;2. Release <strong>of</strong> information documentation;3. Any psychiatric or other advanced directive;4. Legal documentation establishing guardianship;5. Evidence that individual rights are reviewed at least one time a year;6. Evidence that individual responsibilities are reviewed at least one time a year; <strong>and</strong>7. Legal status as it relates to Title 37.vi. Pertinent medical information;vii. Records or reports from previous or other current providers;viii. Correspondence.ix. Frequency <strong>and</strong> style <strong>of</strong> documentation are appropriate to the frequency <strong>and</strong> intensity <strong>of</strong> services, supports,<strong>and</strong> treatment <strong>and</strong> in accordance with the Service Guidelinex. Clear evidence that the services billed are the services provided.xi. Documentation includes record <strong>of</strong> contacts with persons involved in other aspects <strong>of</strong> the individual’s care,including but not limited to internal or external referrals.xii. There is a process for ongoing communication between staff members working with the same individuals indifferent programs, activities, schedules or shifts.2. ASSESSMENTIndividualized services, supports, care <strong>and</strong> treatment determinations are made on the basis <strong>of</strong> an assessment <strong>of</strong> needs with theindividual. The individual must be informed <strong>of</strong> the findings <strong>of</strong> the assessments in a language he or she can underst<strong>and</strong>.A. Assessments must include but are not limited to the following:i. Justification <strong>of</strong> elements which support diagnosis;ii. Summary <strong>of</strong> central themes <strong>of</strong> presenting symptoms/needs <strong>and</strong> precipitating factors;iii. Consumer strengths, needs, abilities, <strong>and</strong> preferences;iv. Individual’s hopes <strong>and</strong> dreams, or personal life goals;v. Individual’s Perception <strong>of</strong> the issue(s) <strong>of</strong> concern;vi. Prior treatment <strong>and</strong> rehabilitation services used <strong>and</strong> outcomes <strong>of</strong> these services;vii. Interrelationship <strong>of</strong> history <strong>and</strong> assessments;viii. Preferences for treatment, consumer choice <strong>and</strong> hopes for recovery;3It is acceptable that the initials can be used for first <strong>and</strong> middle names. The last name must be spelled out <strong>and</strong> each <strong>of</strong> these must correlatewith the names on the license. This is an effort to ensure that a connection can be made between the printed/stamped name on the chart entry<strong>and</strong> a license.FY2013 Provider Manual for Community <strong>Behavioral</strong> <strong>Health</strong> Providers Page 169