PART I - Department of Behavioral Health and Developmental ...
PART I - Department of Behavioral Health and Developmental ...
PART I - Department of Behavioral Health and Developmental ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
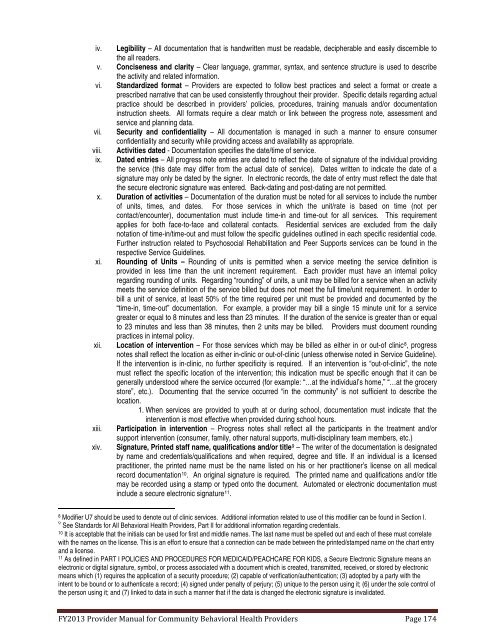
iv. Legibility – All documentation that is h<strong>and</strong>written must be readable, decipherable <strong>and</strong> easily discernible tothe all readers.v. Conciseness <strong>and</strong> clarity – Clear language, grammar, syntax, <strong>and</strong> sentence structure is used to describethe activity <strong>and</strong> related information.vi. St<strong>and</strong>ardized format – Providers are expected to follow best practices <strong>and</strong> select a format or create aprescribed narrative that can be used consistently throughout their provider. Specific details regarding actualpractice should be described in providers’ policies, procedures, training manuals <strong>and</strong>/or documentationinstruction sheets. All formats require a clear match or link between the progress note, assessment <strong>and</strong>service <strong>and</strong> planning data.vii. Security <strong>and</strong> confidentiality – All documentation is managed in such a manner to ensure consumerconfidentiality <strong>and</strong> security while providing access <strong>and</strong> availability as appropriate.viii.ix.Activities dated - Documentation specifies the date/time <strong>of</strong> service.Dated entries – All progress note entries are dated to reflect the date <strong>of</strong> signature <strong>of</strong> the individual providingthe service (this date may differ from the actual date <strong>of</strong> service). Dates written to indicate the date <strong>of</strong> asignature may only be dated by the signer. In electronic records, the date <strong>of</strong> entry must reflect the date thatthe secure electronic signature was entered. Back-dating <strong>and</strong> post-dating are not permitted.x. Duration <strong>of</strong> activities – Documentation <strong>of</strong> the duration must be noted for all services to include the number<strong>of</strong> units, times, <strong>and</strong> dates. For those services in which the unit/rate is based on time (not percontact/encounter), documentation must include time-in <strong>and</strong> time-out for all services. This requirementapplies for both face-to-face <strong>and</strong> collateral contacts. Residential services are excluded from the dailynotation <strong>of</strong> time-in/time-out <strong>and</strong> must follow the specific guidelines outlined in each specific residential code.Further instruction related to Psychosocial Rehabilitation <strong>and</strong> Peer Supports services can be found in therespective Service Guidelines.xi.xii.xiii.xiv.Rounding <strong>of</strong> Units – Rounding <strong>of</strong> units is permitted when a service meeting the service definition isprovided in less time than the unit increment requirement. Each provider must have an internal policyregarding rounding <strong>of</strong> units. Regarding “rounding” <strong>of</strong> units, a unit may be billed for a service when an activitymeets the service definition <strong>of</strong> the service billed but does not meet the full time/unit requirement. In order tobill a unit <strong>of</strong> service, at least 50% <strong>of</strong> the time required per unit must be provided <strong>and</strong> documented by the“time-in, time-out” documentation. For example, a provider may bill a single 15 minute unit for a servicegreater or equal to 8 minutes <strong>and</strong> less than 23 minutes. If the duration <strong>of</strong> the service is greater than or equalto 23 minutes <strong>and</strong> less than 38 minutes, then 2 units may be billed. Providers must document roundingpractices in internal policy.Location <strong>of</strong> intervention – For those services which may be billed as either in or out-<strong>of</strong> clinic 8 , progressnotes shall reflect the location as either in-clinic or out-<strong>of</strong>-clinic (unless otherwise noted in Service Guideline).If the intervention is in-clinic, no further specificity is required. If an intervention is “out-<strong>of</strong>-clinic”, the notemust reflect the specific location <strong>of</strong> the intervention; this indication must be specific enough that it can begenerally understood where the service occurred (for example: “…at the individual’s home,” “…at the grocerystore”, etc.). Documenting that the service occurred “in the community” is not sufficient to describe thelocation.1. When services are provided to youth at or during school, documentation must indicate that theintervention is most effective when provided during school hours.Participation in intervention – Progress notes shall reflect all the participants in the treatment <strong>and</strong>/orsupport intervention (consumer, family, other natural supports, multi-disciplinary team members, etc.)Signature, Printed staff name, qualifications <strong>and</strong>/or title 9 – The writer <strong>of</strong> the documentation is designatedby name <strong>and</strong> credentials/qualifications <strong>and</strong> when required, degree <strong>and</strong> title. If an individual is a licensedpractitioner, the printed name must be the name listed on his or her practitioner’s license on all medicalrecord documentation 10 . An original signature is required. The printed name <strong>and</strong> qualifications <strong>and</strong>/or titlemay be recorded using a stamp or typed onto the document. Automated or electronic documentation mustinclude a secure electronic signature 11 .8Modifier U7 should be used to denote out <strong>of</strong> clinic services. Additional information related to use <strong>of</strong> this modifier can be found in Section I.9 See St<strong>and</strong>ards for All <strong>Behavioral</strong> <strong>Health</strong> Providers, Part II for additional information regarding credentials.10It is acceptable that the initials can be used for first <strong>and</strong> middle names. The last name must be spelled out <strong>and</strong> each <strong>of</strong> these must correlatewith the names on the license. This is an effort to ensure that a connection can be made between the printed/stamped name on the chart entry<strong>and</strong> a license.11As defined in <strong>PART</strong> I POLICIES AND PROCEDURES FOR MEDICAID/PEACHCARE FOR KIDS, a Secure Electronic Signature means anelectronic or digital signature, symbol, or process associated with a document which is created, transmitted, received, or stored by electronicmeans which (1) requires the application <strong>of</strong> a security procedure; (2) capable <strong>of</strong> verification/authentication; (3) adopted by a party with theintent to be bound or to authenticate a record; (4) signed under penalty <strong>of</strong> perjury; (5) unique to the person using it; (6) under the sole control <strong>of</strong>the person using it; <strong>and</strong> (7) linked to data in such a manner that if the data is changed the electronic signature is invalidated.FY2013 Provider Manual for Community <strong>Behavioral</strong> <strong>Health</strong> Providers Page 174